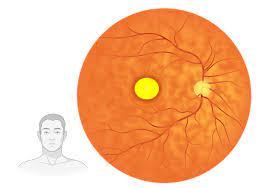
An uncommon, inherited eye condition known as Vitelliform Macular Dystrophy (VMR) affects the macula, the area of the retina in the center of the eye that provides clear central vision. It is frequently described as a “juvenile macular dystrophy” since it frequently shows symptoms in youth or adolescence. VMR is characterized by the buildup of yellowish deposits beneath the macula, known as lipofuscin, which can cause progressive vision loss.
Why It’s Important to Understand Vitelliform Macular Dystrophy?
Understanding VMR is important because it enables sufferers and their families to decide how best to handle the disease. Despite the fact that there is presently no cure for VMR, there are methods and therapies that can assist in decreasing the disease’s progression and enhance the lives of individuals who are affected.
Genetics of Vitelliform Macular Dystrophy
There is a significant genetic component to VMR, and multiple genes have been linked to the disease. The normal functioning of the macula can be interfered with by mutations in these genes, which can result in VMR. For early detection and perhaps future development of targeted therapeutics, it is critical to comprehend the genetics of VMR.
Inheritance Patterns
Autosomal dominant, autosomal recessive, and X-linked inheritance patterns are all possible inheritance patterns for VMR. The most prevalent form of VMR is autosomal dominant, in which case the disorder can be caused by a single copy of the mutant gene. Assessing the likelihood of VMR in upcoming generations can be made easier by understanding the inheritance pattern in a family.
Vitelliform Macular Dystrophy’s Progression
Symptoms and Stages
VMR develops several stages, each of which has its own set of symptoms:
- Pre-Vitelliform Stage: In this early stage, there may be no obvious symptoms, but specialized tests can identify tiny abnormalities in the macula.
- Vitelliform Stage: Yellowish deposits, called vitelliform lesions, build up behind the macula, causing central vision to become distorted or blurry.
- Stage of pseudohypopyon: The vitelliform lesions may reposition, giving the deposits a layer-like appearance.
- Atrophic Stage: The vitelliform lesions may contract and cause the macula to atrophy over time, severely impairing vision.
- End-Stage: In extreme circumstances, the macula may scar and cause severe central vision impairment.
How to Recognize the Warning Signs?
For an early diagnosis and treatment, it is essential to recognize the early signs of VMR, such as changes in central vision or the emergence of vitelliform lesions. For people with a family history of VMR in particular, routine eye exams are essential for spotting these changes.
Risk Factors and Causes
Environmental Elements
VMR is largely inherited, although environmental variables can significantly affect how it develops and progresses. These elements might include smoking, being exposed to certain chemicals, and ultraviolet (UV) light exposure. To protect your eyes, it’s critical to reduce these risks.
Are You at Risk?
It’s important that you understand your VMR risk factors. You may be at a higher risk if you have a family history of the disorder or carry known genetic variants linked to VMR. Regular eye exams will help you keep track of your eye health and, if VMR develops, can find it early.
Vitelliform Macular Dystrophy Diagnosis
The Importance of Early Diagnosis
Implementing solutions to stop VMR’s progression and protect vision depends on an early diagnosis. Vitelliform lesions and other VMR-related alterations can be found early with routine eye exams, including dilated fundus checks and imaging methods like optical coherence tomography (OCT).
Diagnostic Procedures
To confirm the diagnosis and determine the severity of VMR, further diagnostic methods, such as electroretinography (ERG) and genetic testing, may be used in addition to fundus examinations and OCT. Genetic testing is useful for locating certain mutations linked to the illness.
Best Disease, A VMR Subtype
What Distinguishes Best Disease?
Best Disease is a particular kind of VMR also known as vitelliform macular dystrophy type 2 (VMD2). Compared to other types of VMR, it has a more regular and recognizable pattern of growth. Accurate diagnosis and treatment can benefit from an understanding of the variations between Best Disease and other VMR subtypes.
The Differences
Best Disease often manifests as clearly defined vitelliform lesions and progresses more steadily. Other types of VMR, however, may appear differently and proceed at varying speeds. Even though the underlying genetic abnormalities are connected, the clinical characteristics can vary greatly.
Treatment Options
Although there is no treatment for VMR or Best Disease, there are ways to manage the condition and perhaps even slow down its development. These may consist of:
- Intravitreal injections of anti-VEGF drugs can aid in reducing the development of abnormal blood vessels and fluid leaking, two symptoms that can be related to VMR.
- Low vision aids can help people with VMR make the most of their remaining vision. Examples include magnifiers and telescopic lenses.
- Genetic Therapies: Genetic therapies for VMR are now being researched, with the hope of addressing the underlying genetic origins of the disorder.
Latest Therapies
The study of innovative therapies and interventions is an active area in the field of VMR research. These might include techniques for gene therapy that try to fix particular genetic mutations that cause VMR. Keep abreast of the most recent findings, and get advice from a retinal specialist on any potential clinical studies.
Making use of an Amsler Grid
What It Does
A straightforward technique for tracking changes in central vision is the Amsler Grid. It is made up of a grid of straight lines with a dot in the middle. This grid can be used by people with VMR to find any distortions or blank spots in their center vision.
Benefits for Patients with VMR
The Amsler Grid enables people with VMR to regularly monitor changes in their vision and notify their healthcare practitioner of any noteworthy changes. To help protect eyesight, early detection of abnormalities can lead to rapid interventions and therapies.
Modifying Your Lifestyle to Manage VMR
Nutrition and Diet
Certain nutrients are necessary for maintaining the health of the macula, and dietary decisions can have an impact on eye health. Think about including foods high in zinc, omega-3 fatty acids, antioxidants, vitamins A, C, and E in your diet. These vitamins and minerals promote retinal health and may slow the development of VMR.
Protecting Your Eyes
It’s important to shield your eyes from environmental hazards like UV rays. When outdoors, put on UV-protective eyewear and stay away from smoking and hazardous chemicals. Maintaining a healthy lifestyle can help you keep your remaining vision.
Managing Vitelliform Macular Dystrophy-Related Vision Loss
Services for Low Vision
Living with VMR can be difficult, but low vision services can significantly improve the quality of life for those who are affected. Low vision specialists can offer individualized evaluations and suggestions for aids and methods to improve daily life.
Assisted Technologies
People with VMR can keep their independence using a variety of assistive technologies. These include screen readers, handheld video magnifiers, electronic reading devices, and magnifiers. Low vision experts can assist you in making the best decision for your needs.
Coping Techniques
Emotionally difficult things can come with coping with visual loss. To assist individuals and their families in navigating the emotional aspects of living with VMR, support groups, and counseling services are offered. Developing resilience and learning adaptive skills can both be quite beneficial.
Other Macular Dystrophies
A collection of inherited eye conditions known as macular dystrophies primarily damages the macula, the region of the retina that is crucial for clear central vision. Other macular dystrophies, like Vitelliform Macular Dystrophy (VMR), can cause vision loss and central visual impairment. Here are several other macular degenerations:
One of the most prevalent types of juvenile macular dystrophy is Stargardt disease, also known as Stargardt macular dystrophy. The retinal pigment epithelium (RPE) gradually accumulates lipofuscin, which is characteristic of the condition, and often starts in childhood or adolescence. This results in loss of central vision and frequently in legal blindness.
Pattern Dystrophy
The macula is affected in a particular pattern by a category of uncommon macular dystrophies known as pattern dystrophies. There are numerous subtypes, including reticular dystrophy, butterfly-shaped pigment dystrophy, and adult-onset foveomacular vitelliform dystrophy. Each subtype has distinct pigmentation patterns and visual characteristics.
Cone Dystrophy
The cone cells in the retina, which are in charge of color vision and central visual acuity, are the primary targets of cone dystrophies. Reduced color vision, reduced visual acuity, and increased photosensitivity are frequent effects of these dystrophies.
Cone-Rod Dystrophy
This type of dystrophy, which affects both cone and rod cells in the retina, is more severe. Typically, it causes night blindness and diminished central vision, which are early-onset vision issues.
Best Disease (Best Vitelliform Macular Dystrophy)
The best disease is a particular subtype of macular dystrophy marked by vitelliform lesions, comparable to VMR, as was discussed in the previous blog post. It frequently develops during childhood or adolescence and can compromise central vision.
North Carolina Macular Dystrophy (MCDR1) is a rare autosomal dominant condition that mostly affects residents of that state in the United States. It can cause legal blindness and is characterized by central vision loss.
SFD, or Sorsby Fundus Dystrophy
An autosomal dominant macular dystrophy called Sorsby fundus dystrophy often strikes people in their mid-adult years. Due to the growth of drusen and macular degeneration, it causes a gradual loss of central vision.
Malattia Leventinese, also known as Doyne Honeycomb Dystrophy, is another autosomal dominant macular dystrophy that frequently manifests in adolescence. The development of yellowish deposits (drusen) beneath the macula, which can impede central vision, is what distinguishes it.
Bull’s Eye Maculopathy
This macular dystrophy is frequently linked to drugs like chloroquine or hydroxychloroquine, which are used to treat autoimmune diseases and conditions like malaria. It results in central vision loss and a recognizable “bull’s eye” pattern of pigmentation.
Macular dystrophy similar to that found in North Carolina (MCDR3): Like North Carolina macular dystrophy, this condition affects people differently and has the potential to impair central vision.
Conclusion
To sum up, Vitelliform Macular Dystrophy is a complicated hereditary disorder that necessitates early discovery and a multidisciplinary therapeutic strategy. Even though there is currently no cure, continuous research shows promise for potential future treatments. People with VMR can keep their vision by changing their lifestyles and using technologies like the Amsler Grid. Additionally, assistive technology and low vision services provide a sense of hope and workable solutions for raising quality of life.
FAQs -Common questions regarding VMR
Is VMR curable?
VMR is not currently curable. The goal of treatment is to control the illness and stop its progression.
Is VMR inherited?
Yes, there is a genetic component to VMR, and it can be inherited in a variety of ways, including X-linked heredity, autosomal dominant inheritance, and autosomal recessive inheritance.
Do there exist any dietary suggestions for VMR?
A diet high in antioxidants, vitamins A, C, and E, zinc, and omega-3 fatty acids may promote retinal health and decrease the development of VMR, according to the answer.
What are low vision services and how might they be of assistance?
Low vision services include individualized evaluations, suggestions for aids, and methods to help people with VMR make the most of their remaining eyesight.
Are there any VMR therapy clinical trials underway?
Yes, clinical trials looking into potential treatments for VMR are part of current research. For information on available trials and their eligibility requirements, speak with a retinal specialist.
We have covered every aspect of Vitelliform Macular Dystrophy in this extensive guide, including its genetic basis, diagnosis, course of therapy, and the crucial function of low vision services. Individuals and families impacted by VMR can better traverse this difficult road and look toward the future with optimism and improved vision by arming themselves with knowledge and seeking help.