Learn about Diabetic Retinopathy stages, symptoms and everything that can go wrong with Diabetic eye problems
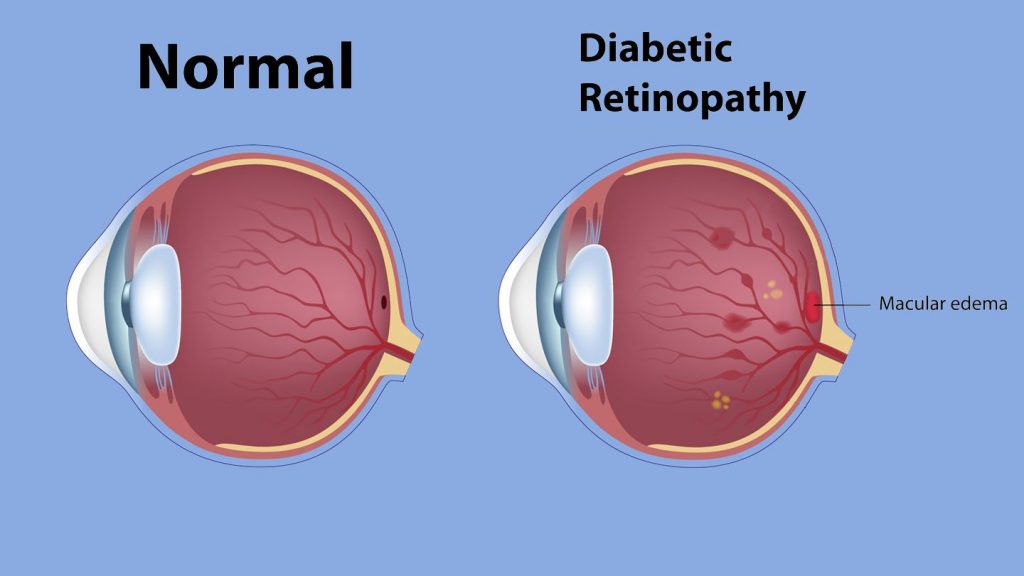
Diabetic retinopathy is an eye disorder that causes the blood vessels in your retina to become weaker.
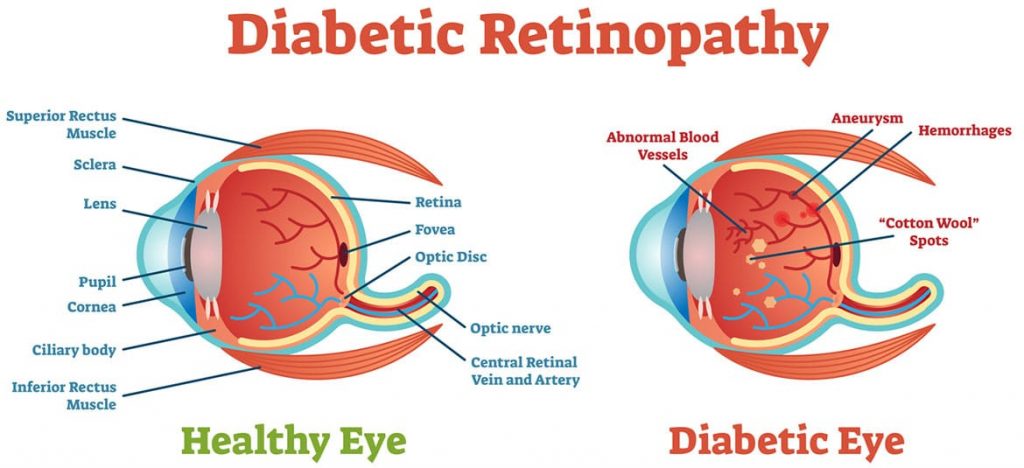
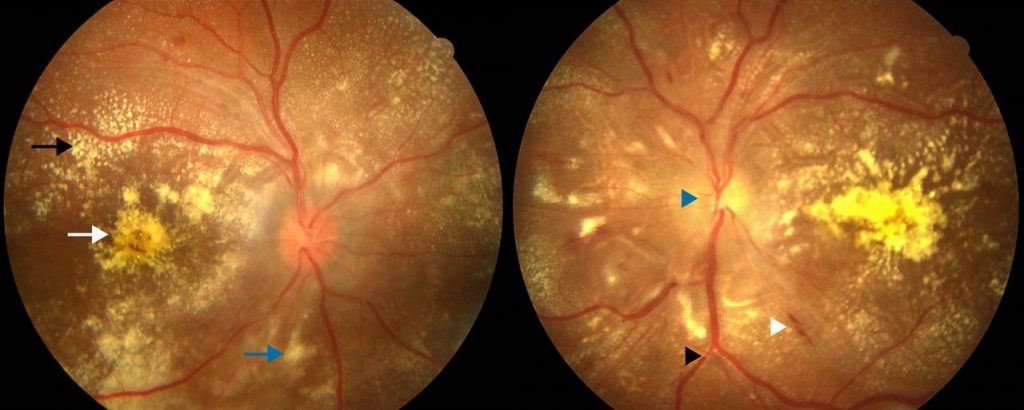
Changes in the blood vessels of the retina, the light-sensitive layer of tissue at the back of the inner eye, produce diabetic retinopathy. The blood vessels in the retina of some patients with diabetic retinopathy may enlarge and leak fluid. In others, aberrant new blood vessels form on the retina’s surface.
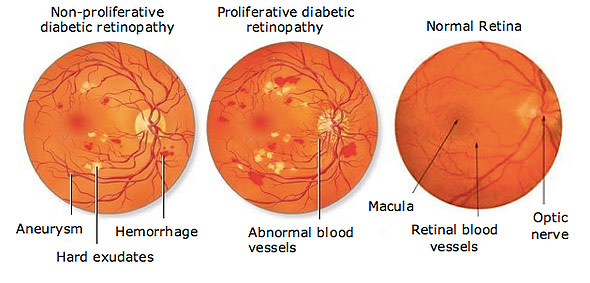
Diabetic retinopathy is classified into two types:
You might have diabetic retinopathy and be completely unaware of it. This is due to the fact that it often exhibits no symptoms in its early stages. As diabetic retinopathy worsens, you may experience symptoms such as:
Symptoms of diabetic retinopathy commonly affect both eyes.
Although retinopathy may be caused by a variety of medical diseases (e.g., sickle cell disease, lupus), diabetes and hypertension are the most frequent (high blood pressure).
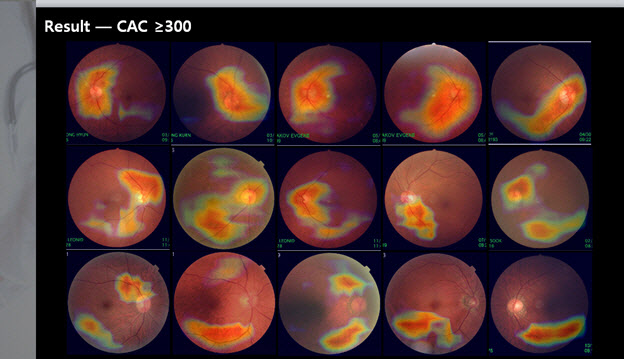
A dilated eye exam is the most accurate approach to identify diabetic retinopathy. During this test, the physician inserts drops in the eyes to dilate (open wide) the pupils, allowing a clearer view of the interior of the eye, particularly the retinal tissue.
The following are the things the doctor will check for:
Diabetic retinopathy may affect people with type 1 or type 2 diabetes.
You’re more at danger if:

New blood vessel development may create retinal scar tissue. Scar tissue shrinkage may distort and pull the retina out of position. 4
A little piece of the retina may be detached with no symptoms. However, a bigger amount removed may cause:

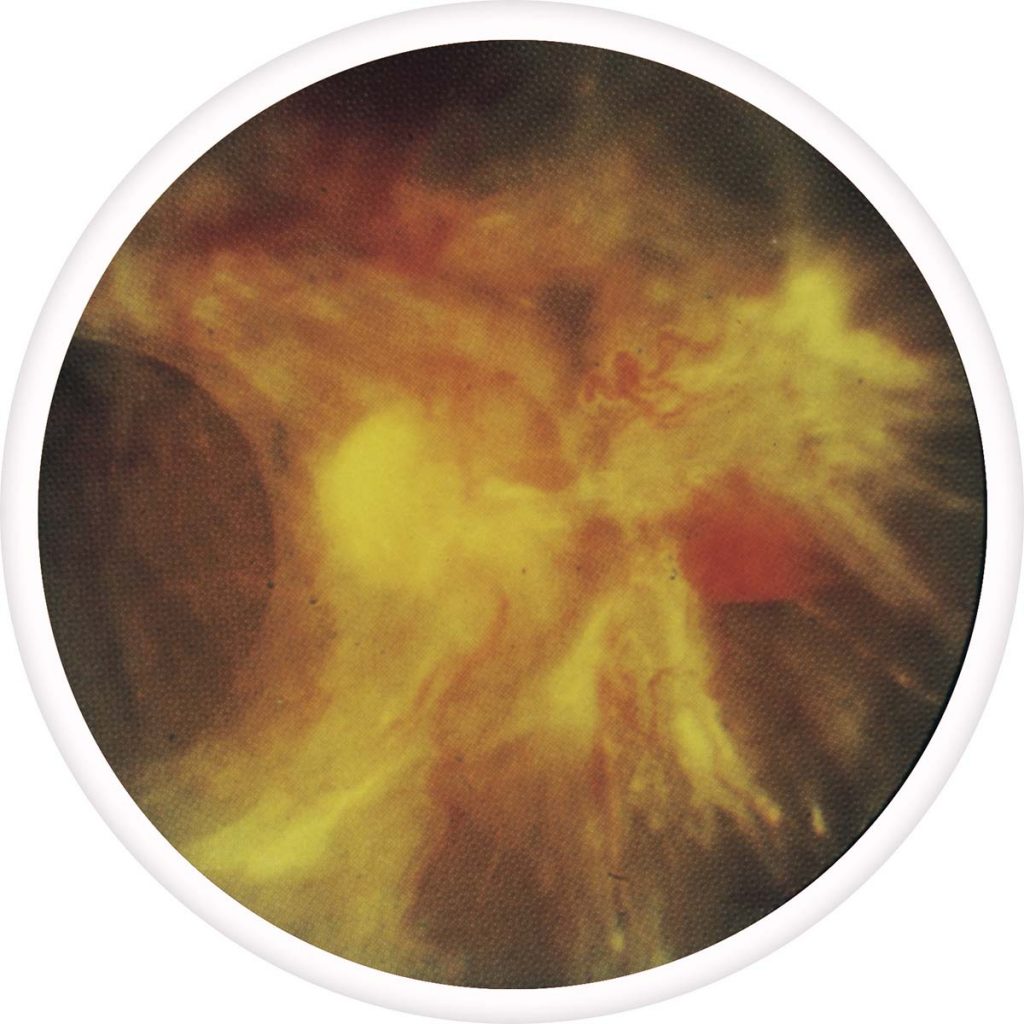
If you do not treat it right away you may end up with a severe condition. Diabetic retinopathy is characterized into four stages: mild, moderate, severe nonproliferative, and proliferative.


Nearly one out of every three diabetics will develop retinopathy, which is damage to the blood vessels in the retina. That’s the line behind your eye. The most common kind of retinopathy is non-proliferative retinopathy, which does not generally endanger your vision.
Diabetes patients with Type 1 and Type 2 diabetes are at a higher risk of ocular problems and blindness. Diabetes-related vision loss, on the other hand, is not unavoidable. Increasing your understanding of vision health and practicing preventive measures will help you keep your eyesight for many years to come.
Preventing Diabetic Eye Disease in 5 Easy Steps
Visit a low vision specialist to learn more about low vision aids and choose the proper ones. Find one in your region.