Learn about types of Glaucoma, symptoms, and the help you can get to address the disease
Glaucoma is a disorder that destroys the optic nerve in your eye. It worsens with time. It’s often associated with an increase in intraocular pressure. Glaucoma is a disease that runs in families. You normally don’t get it till you’re older.
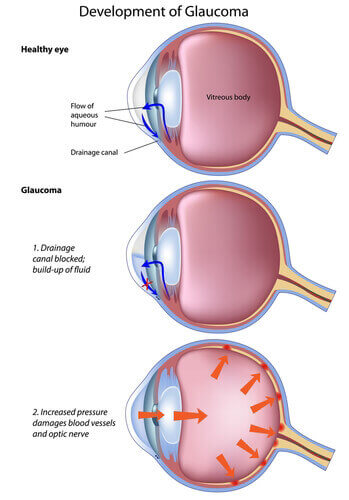
Increased intraocular pressure, often known as glaucoma, may harm your optic nerve, which delivers pictures to your brain. Glaucoma, if left untreated, may cause irreversible vision loss or perhaps complete blindness within a few years.
Lowering your eye pressure might help you retain your vision. Most glaucoma patients who adhere to their treatment plan and have frequent eye examinations are able to maintain their vision.
For those over the age of 60, glaucoma is one of the major causes of blindness. It may happen at any age, although it is more frequent in elderly people.
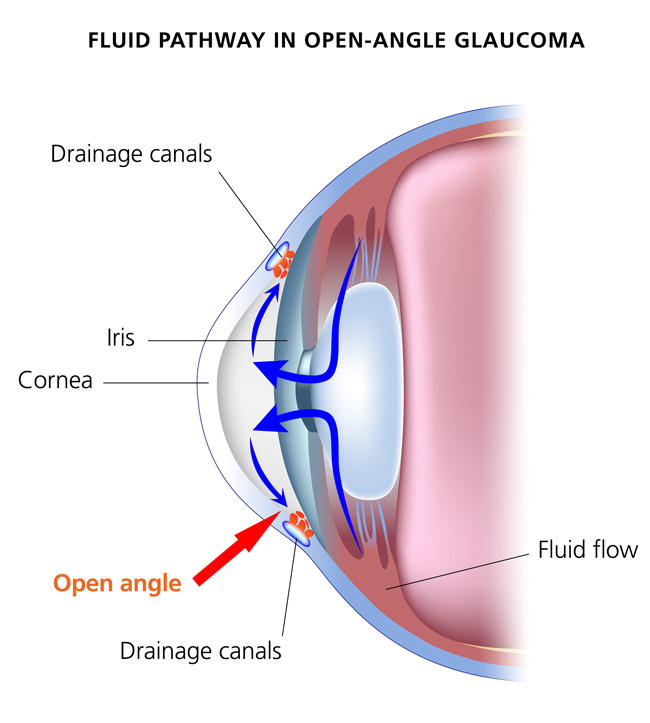
Open-Angle Glaucoma: The most prevalent kind of glaucoma, accounting for at least 90% of all glaucoma cases, is caused by the gradual blockage of drainage tubes, resulting in increasing eye pressure.
Angle-Closure Glaucoma: Angle-closure glaucoma is a less frequent kind of glaucoma characterized by clogged drainage canals, resulting in an abrupt increase in intraocular pressure.
Glaucoma with Normal Tension (NTG): Low-tension glaucoma is sometimes known as normal-tension glaucoma. Even though the eye pressure is not extremely high in normal-tension glaucoma, the optic nerve is injured.
Congenital glaucoma: This kind of glaucoma develops in neonates when the drainage canals of the eye do not develop properly or at all during the prenatal period. This is an uncommon disorder that may be passed down through families.
Other types of glaucoma include:
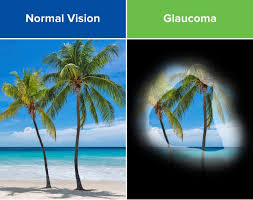
Open-angle glaucoma symptoms usually appear gradually and subtly. As a result, they are simple to overlook. Many patients with open-angle glaucoma have no apparent symptoms at first, making frequent eye examinations critical for detecting this illness in its early stages. Because glaucoma damage is permanent, early identification and treatment are critical for avoiding blindness.
Closed-angle glaucoma symptoms are more severe and tend to appear abruptly.
You may encounter the following symptoms with any type:
Glaucoma may develop for a variety of causes.
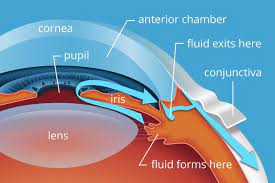
The majority of instances are caused by a buildup of pressure in the eye produced by fluid that is unable to drain normally.
The nerve that links the eye to the brain is then damaged as a result of the rise in pressure (optic nerve).
It’s not always apparent why this occurs, although some factors might raise the risk, such as:
your age – glaucoma gets more prevalent as you grow older your race – persons of African, Caribbean, or Asian descent are more likely to develop it
your family history – if you have a parent or sibling who has glaucoma, you are more likely to get the disease other medical issues – such as short-sightedness, long-sightedness, and diabetes
It is unclear if there is anything you can do to avoid glaucoma, but frequent eye exams should detect it as early as feasible.
A tonometer measures the pressure within your eye during an eye pressure test (tonometry).
A gonioscopy examines the fluid-filled gap between the colored component (iris) and the clear window at the front of the eye (cornea). This is where your eye fluid should drain.
A visual field test (perimetry) looks for blind spots.
The optic nerve, which links your eye to your brain, may be affected by glaucoma; thus, it may be tested.
a scan that uses specific light beams to image the retina.
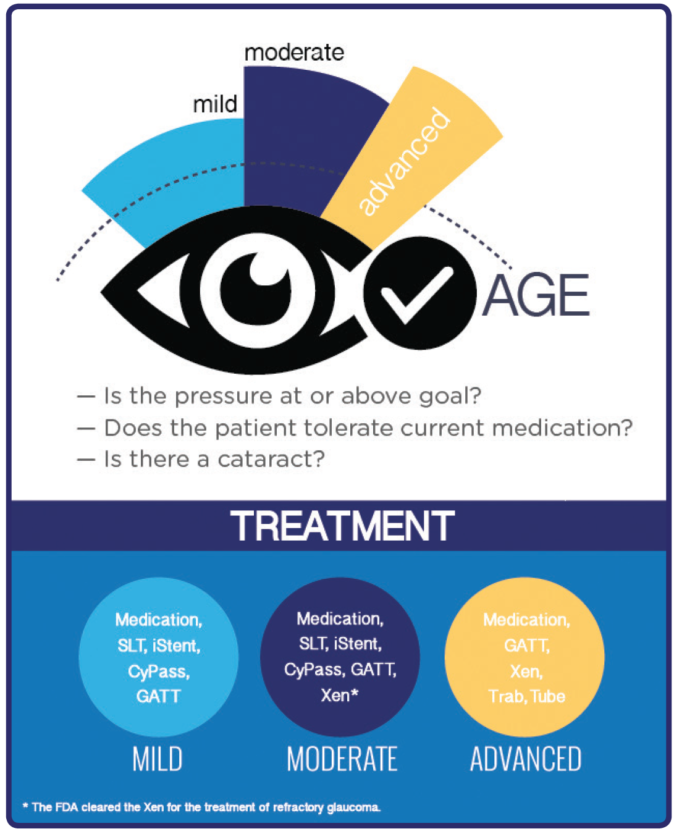
Treatments include:
Glaucoma and its consequences should be of concern to everyone.
People who are more vulnerable:


Acute angle-closure glaucoma is an eye emergency because it may cause irreparable blindness if not detected and treated promptly. You may feel or get ill (vomit). Immediate therapy is required to alleviate symptoms and avoid irreversible visual loss (severe sight impairment).
Acute glaucoma is characterized by a sudden restriction of the outflow of aqueous humour fluid from your eye. As more fluid is produced, the pressure within your eye rapidly increases. This may cause damage to the optic nerve in the back of the eye, impairing vision.
Symptoms generally appear all of a sudden. They are as follows:
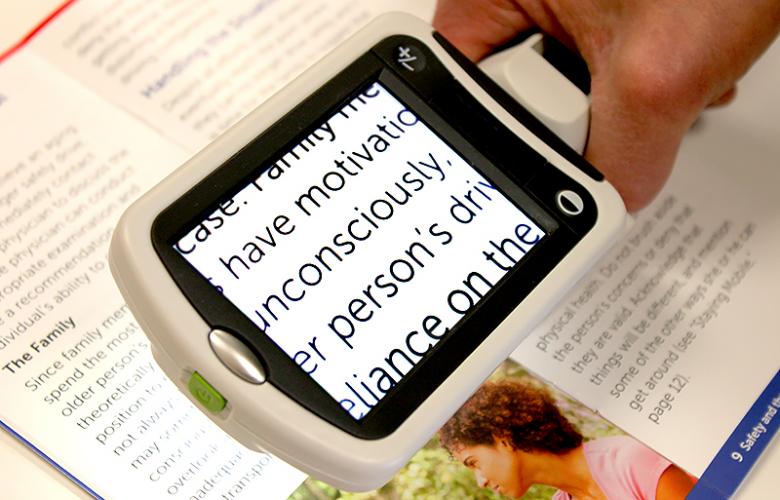
Low vision devices may enhance your quality of life without being electrical or very technological.

If you do not treat your glaucoma, your eyesight will deteriorate. Patients usually lose their peripheral vision first, followed by a narrowing of their center vision. Patients who do not manage their glaucoma symptoms may eventually lose their eyesight and become blind. At this stage, patients may need to explore solutions like as a service animal or a blind cane to move about without their sight. This is avoidable with good glaucoma treatment in Yakima.
Glaucoma is treatable, particularly if detected early. Yakima Vision Center’s Optometrist can help delay the advancement of the condition, allowing you to keep more of your vision for longer. There are several treatment options for glaucoma, and we would be pleased to discuss them with you during a consultation.
After completing his or her residency, a “Board Certified” Ophthalmologist must pass both a written and oral test. During the oral exam, a small panel of professional ophthalmologists question the doctor how he or she would manage particular scenarios during surgery. A Board Certified Ophthalmologist has the experts’ stamp of approval, giving patients peace of mind that their doctor is an expert in Ophthalmology.
Glaucoma may be detected and treated by an optometrist or a conventional ophthalmologist. A glaucoma specialist, on the other hand, has greater glaucoma training and a broader selection of treatment options for their patients.
An ophthalmologist must first finish four years of medical school, followed by four years of residency training. Following residency, the doctor is eligible to take the Ophthalmology professional licensing test. An ophthalmologist can identify and treat glaucoma, but physicians who want to understand how to treat advanced, severe, rare, or difficult types of glaucoma might complete extra training known as a fellowship. Most crucially, in order to be competent as a glaucoma surgeon, a glaucoma specialist must undertake a lot of genuine glaucoma procedures.


Glaucoma may strike at any age. That doesn’t imply everyone is at danger.
Visit a low vision specialist to learn more about low vision aids and choose the proper ones. Find one in your region.