Diabetic retinopathy is a complication of diabetes that affects the eyes. It occurs when high blood sugar levels damage the blood vessels in the retina. The first sign of diabetic retinopathy is often no symptoms at all, which is why it is important for people with diabetes to have regular eye exams. However, as the condition progresses, the following symptoms may appear:
- Blurred or distorted vision
- Difficulty seeing at night
- Dark spots or empty areas in the vision
- Flashes of light or floaters in the vision
- Eye pain or pressure
If you have diabetes, it is important to have regular eye exams, even if you do not have any symptoms of diabetic retinopathy. Early detection and treatment of diabetic retinopathy can help prevent or slow down vision loss.
Overview
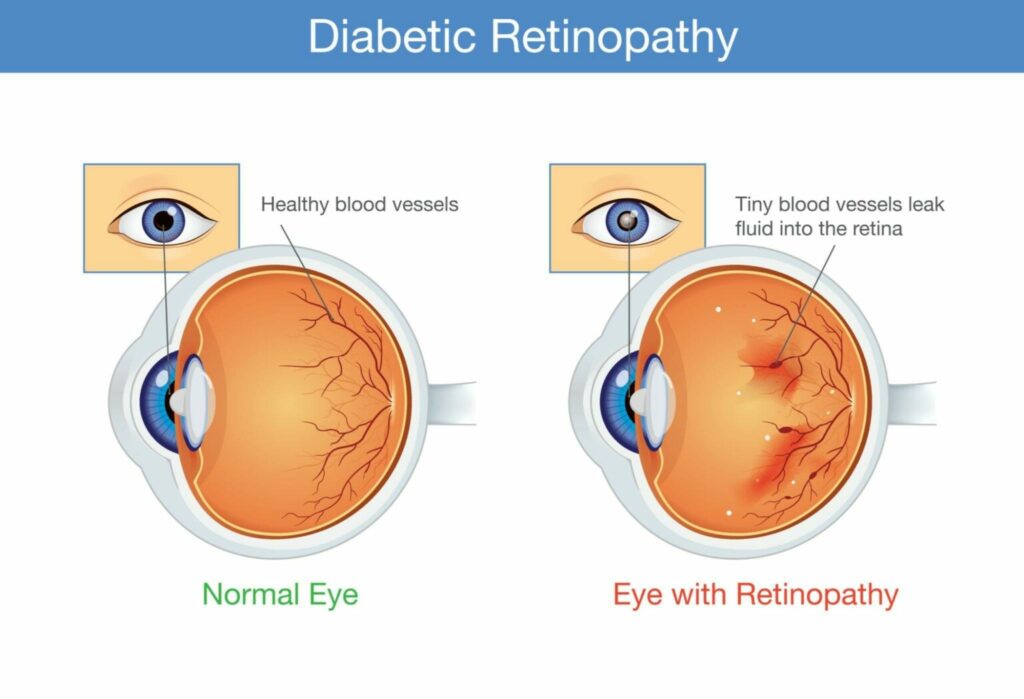
Diabetes complications that damage the eyes are referred to as diabetic retinopathy (die-uh-BET-ik reti-NOP-uh-thee). Damage to the blood vessels in the light-sensitive tissue (the retina) in the back of the eye is what causes it.
Initially, diabetic retinopathy may not manifest any symptoms or may only result in minor vision issues. Yet it could result in blindness.
Each person with type 1 or type 2 diabetes has the potential to acquire the illness. The likelihood of developing this ocular problem increases with the duration of diabetes and the degree of blood sugar management.
How often should I have an eye exam if I have diabetes?
If you have diabetes, it is recommended to have a comprehensive eye exam at least once a year. This is because diabetic retinopathy can develop without any noticeable symptoms in its early stages, and an eye exam can detect the condition before it progresses and causes vision loss.
In some cases, your eye doctor may recommend more frequent eye exams if you have signs of diabetic retinopathy or if you have other risk factors for eye complications, such as high blood pressure or kidney disease.
It is important to follow the recommendations of your eye doctor and have regular eye exams as part of your diabetes management plan. Additionally, it is essential to maintain good blood sugar control, blood pressure control, and other diabetes management strategies to help reduce the risk of developing diabetic retinopathy and other diabetes-related complications.
How is it diagnosed?
Diabetic retinopathy is typically diagnosed during a comprehensive eye exam that includes several tests to evaluate the health of the eyes. These tests may include:
Visual acuity test
This test measures how well you can see at various distances using an eye chart.
Dilated eye exam
During this exam, your eye doctor will use eye drops to dilate your pupils, which allows them to examine the retina and optic nerve for any signs of damage or disease.
Tonometry
This test measures the pressure inside your eyes.
Fluorescein angiography
This test involves injecting a dye into your arm and taking pictures of the blood vessels in your eye as the dye passes through them. This can help identify any abnormal blood vessels or areas of leakage.
Optical coherence tomography (OCT)
This test uses light waves to create detailed images of the retina, allowing your eye doctor to detect any swelling or fluid buildup.
Based on the results of these tests, your eye doctor will be able to determine if you have diabetic retinopathy and how severe it is. If you are diagnosed with diabetic retinopathy, your eye doctor may recommend further testing or treatment to help manage the condition and prevent vision loss.
Is retinopathy painful?
In general, diabetic retinopathy is not a painful condition. However, as the condition progresses, you may experience some discomfort or pain in your eyes, especially if there is swelling or fluid buildup in the retina.
In some cases, diabetic retinopathy can cause the growth of new blood vessels in the retina, which can lead to bleeding and scarring. This can cause symptoms such as blurred or distorted vision, floaters in the vision, and, in rare cases, sudden vision loss. However, these symptoms are typically not associated with pain.
If you are experiencing any discomfort or pain in your eyes, it is important to see your eye doctor to determine the underlying cause and receive appropriate treatment.
What causes diabetic retinopathy?
Diabetic retinopathy is caused by high blood sugar levels that damage the blood vessels in the retina, which is part of the eye that senses light and sends visual signals to the brain. Over time, high blood sugar levels can cause the blood vessels in the retina to become weakened and leaky, or to close off completely, preventing blood from reaching the retina.
As the condition progresses, new blood vessels may grow in the retina, but these new vessels are often weak and prone to bleeding, which can cause further damage to the retina and lead to vision loss.
Several factors can increase the risk of developing diabetic retinopathy, including:
- Poor blood sugar control
- High blood pressure
- High cholesterol levels
- Smoking
- Diabetes duration
- Pregnancy
- Kidney disease
It is important to manage these risk factors and control blood sugar levels to help reduce the risk of developing diabetic retinopathy and other diabetes-related complications. Additionally, regular eye exams can help detect diabetic retinopathy early, before it causes significant vision loss.
What are the stages of retinopathy?
There are two main stages of diabetic retinopathy:
Non-proliferative diabetic retinopathy (NPDR)
This is the early stage of diabetic retinopathy and is characterized by small areas of swelling in the retina, called microaneurysms, as well as leaking blood vessels and fluid buildup. In some cases, there may be areas of decreased blood flow to the retina. Most people with NPDR do not experience any symptoms, but if left untreated, the condition can progress to proliferative diabetic retinopathy.
Proliferative diabetic retinopathy (PDR)
This is the more advanced stage of diabetic retinopathy and is characterized by the growth of new blood vessels in the retina. These new blood vessels are fragile and prone to bleeding, which can cause vision loss. Additionally, the new blood vessels can cause scar tissue to form, which can pull on the retina and cause it to detach. Symptoms of PDR can include blurred or distorted vision, floaters in the vision, and, in rare cases, sudden vision loss.
It is important to have regular eye exams to detect diabetic retinopathy early before it progresses to the more advanced stages and causes vision loss. Treatment options are available for both NPDR and PDR to help manage the condition and prevent or slow down vision loss.
What groups are most at risk?
Several groups are considered to be at higher risk for developing diabetic retinopathy:
People with diabetes
People with type 1 or type 2 diabetes are at the highest risk for developing diabetic retinopathy.
People with poor blood sugar control
Poor blood sugar control can increase the risk of developing diabetic retinopathy, as high blood sugar levels can damage the blood vessels in the retina.
People with high blood pressure
High blood pressure can damage the blood vessels in the retina, increasing the risk of developing diabetic retinopathy.
People with high cholesterol levels
High levels of cholesterol in the blood can cause the buildup of plaque in the blood vessels, which can damage the blood vessels in the retina.
Smokers
Smoking can increase the risk of developing diabetic retinopathy, as well as other diabetes-related complications.
Pregnant women with diabetes
Pregnancy can increase the risk of developing diabetic retinopathy, particularly for women with pre-existing diabetes.
People with kidney disease
Kidney disease is a common complication of diabetes and can increase the risk of developing diabetic retinopathy.
It is important for people in these high-risk groups to have regular eye exams to detect diabetic retinopathy early before it causes significant vision loss. Additionally, managing diabetes and other risk factors can help reduce the risk of developing diabetic retinopathy and other diabetes-related complications.
Diabetic retinopathy can cause several complications, including:
Vision loss
The most common complication of diabetic retinopathy is vision loss. This can occur as a result of bleeding in the retina, swelling, or detachment of the retina.
Macular edema
Diabetic retinopathy can cause fluid to accumulate in the macula, which is the central part of the retina responsible for sharp, detailed vision. This can cause blurred or distorted vision.
Neovascular glaucoma
In some cases, new blood vessels can grow in the front part of the eye, blocking the flow of fluid out of the eye and causing increased pressure, which can lead to neovascular glaucoma. This is a rare but serious complication that can cause permanent vision loss if not treated promptly.
Retinal detachment
Diabetic retinopathy can cause scar tissue to form in the retina, which can pull on the retina and cause it to detach from the back of the eye. This can cause sudden vision loss and requires immediate medical attention.
Blindness
If left untreated, diabetic retinopathy can progress to advanced stages and cause permanent vision loss or blindness.
It is important to have regular eye exams to detect diabetic retinopathy early and to manage the condition to prevent or slow down vision loss and other complications. Treatment options are available to help manage diabetic retinopathy and prevent vision loss.
Can Diabetic retinopathy be prevented?
While diabetic retinopathy cannot be completely prevented, there are steps that people with diabetes can take to reduce their risk of developing the condition and to help prevent it from progressing:
Control blood sugar levels
One of the most important ways to prevent diabetic retinopathy is to maintain good control of blood sugar levels. This can help reduce the damage to blood vessels in the retina.
Control blood pressure and cholesterol levels
High blood pressure and cholesterol levels can also contribute to the development of diabetic retinopathy, so it is important to manage these conditions as well.
Have regular eye exams
People with diabetes should have regular eye exams to detect diabetic retinopathy early before it causes significant vision loss. The American Diabetes Association recommends annual eye exams for people with diabetes.
Follow a healthy lifestyle
Eating a healthy diet, getting regular exercise, and not smoking can also help reduce the risk of developing diabetic retinopathy.
Take medication as prescribed
People with diabetes should take their medications as prescribed and follow their doctor’s instructions to manage their condition effectively.
While these steps can help reduce the risk of developing diabetic retinopathy, it is important to remember that people with diabetes are still at higher risk for the condition and should have regular eye exams to detect and manage it early.
What is the treatment for early diabetic retinopathy?
The treatment for early diabetic retinopathy depends on the specific condition and its severity. In many cases, early diabetic retinopathy can be managed by controlling blood sugar, blood pressure, and cholesterol levels, and by having regular eye exams to monitor the condition.
If macular edema is present, the doctor may recommend treatment with medications called anti-VEGF drugs, which can help reduce swelling in the macula and improve vision. These medications are typically injected into the eye.
If proliferative diabetic retinopathy is present, laser surgery may be recommended to help reduce the growth of abnormal blood vessels in the retina. This type of surgery is called panretinal photocoagulation (PRP) and involves using a laser to create small burns in the retina, which can help reduce the growth of abnormal blood vessels.
If diabetic retinopathy is detected early, the goal of treatment is to prevent it from progressing to more advanced stages that can cause permanent vision loss or blindness. It is important to have regular eye exams and to work closely with your doctor to manage your diabetes and other health conditions effectively.
Conclusion
As mentioned multiple times above, the key to managing early diabetic retinopathy signs is to have regular eye exams. This can not be stressed enough, also healthy eating and lifestyle along with regular visits to your doctor.
FAQ’s
What may be misdiagnosed as diabetic retinopathy?
Patients with diabetes may experience a variety of common ocular and systemic diseases that resemble diabetic retinopathy (136).
- Macular degeneration is brought on by aging.
- Retinopathy brought on by hypertension.
- Radiation-induced retinopathy.
- Other reasons for retinopathy.
Is diabetic retinopathy reversible?
Treatment can not cure diabetic retinopathy, although it can delay or stop its development. Future retinal degeneration and vision loss are still likely due to diabetes’ lifetime nature. You’ll need routine eye exams even if your diabetic retinopathy has been treated. You could eventually require more care.
How soon does retinopathy result from diabetes?
Patients with diabetes often experience the onset of diabetic retinopathy three to five years after being diagnosed with the disease. Although diabetic retinopathy won’t initially impair vision, if it is left untreated it will eventually cause vision loss.