The Difference Between Wet and Dry AMD
People living with wet AMD could benefit from injectable drugs that block growth factors that cause abnormal blood vessels to grow and leak, according to new studies.
Your physician will use fluorescein angiography and optical coherence tomography (OCT) to monitor what’s going on with your retina, including testing called Amsler grid that helps identify any early changes in central vision.
Treatment for Dry AMD
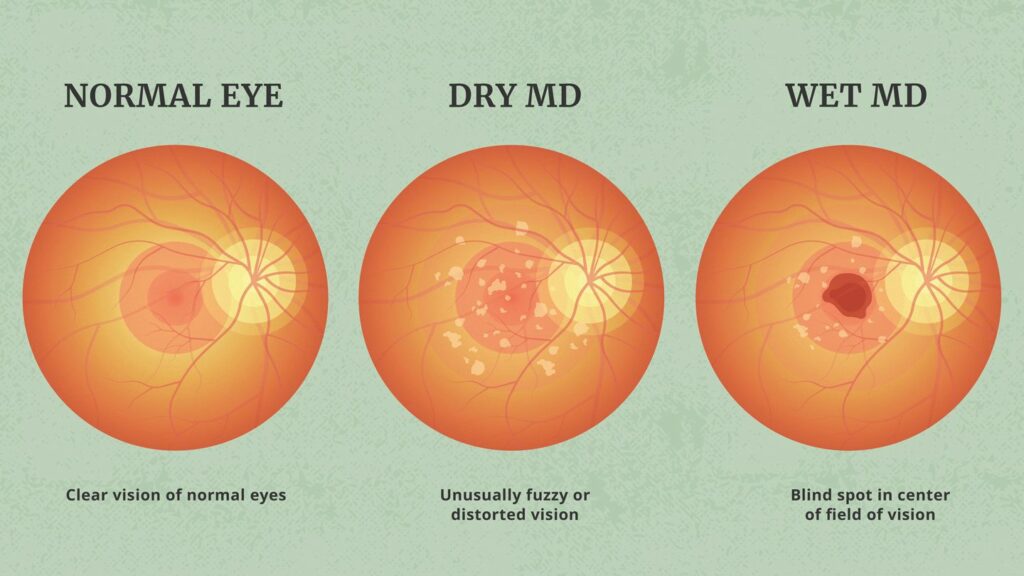
Dry AMD often takes years to develop, and usually affects both eyes. With this form of AMD, small protein clumps (drusen) accumulate under the retina that lines the back of your eyeball. Over time, drusen causes macular thickness to decrease, making it harder to see straight lines and objects clearly and sometimes leaving an ’empty spot’ in your central vision. Luckily, it doesn’t lead to blindness as peripheral vision (which allows us to see objects around us) is unaffected.
Wet macular degeneration (WMD), a less prevalent but more serious form of AMD, occurs when abnormal blood vessels sprout beneath the retina and leak fluid, damaging retinal cells rapidly and leading to rapid central vision loss. Unfortunately, WMD can be more challenging to treat than dry AMD; however there have been clinical trials conducted of promising therapies.
Study conducted by UT Southwestern ophthalmologists revealed that taking specific vitamins could halt the progression of dry AMD into wet macular degeneration. The AREDS2 trial included 4,200 patients who received either antioxidant and zinc supplements, fish oil capsules or placebo treatments; researchers discovered this combination slowed visual loss by about 25%; it is recommended for all early or intermediate dry AMD sufferers taking an AREDS2 supplement daily for optimal outcomes.
Other methods used to prevent wet AMD from developing include laser surgery and injections of an anti-VEGF medication. With laser treatment, high energy beams of light destroy fragile blood vessels causing wet AMD. Reduce or stop the flow of fluid under the retina to help protect against further macula damage and restore some vision loss. However, this treatment option only works for limited number of individuals suffering from wet AMD, and repeated treatments must be administered over time for it to have any lasting effects. An intravitreal injection of a drug that targets and destroys abnormal blood vessels could also help combat wet macular degeneration; further research will be necessary to assess its efficacy and safety.
Treatment for Drusen
Macular degeneration’s dry form occurs as people age, when tiny clumps of protein called drusen begin to appear in their retinas. Drusen don’t cause vision loss directly but are an indicator that light sensitive tissues in your eye have begun breaking down, leading to blurry spots in central vision which become larger and darker over time. At root level this problem stems from retina losing its ability to transmit signals directly to the brain where interpretation takes place resulting in images being created by brain.
At least eight out of 10 people living with AMD experience its dry form, which occurs when their macula breaks down or thins due to formation of drusen – tiny yellow deposits under the retina that don’t cause vision loss directly; as more and larger drusen form under their retinas they can lead to thinner maculae and less effective functioning overall.
People suffering from dry AMD often reach the early stage (intermediate macular degeneration) before they notice any noticeable blurring in their central vision. At this stage, additional lighting may be required to improve visibility; eye health professionals can assess an individual’s risk for advanced AMD by testing with an Amsler grid or imaging tests.
Early on in a disease’s course, drusen can be divided into two distinct categories; hard and soft drusen. Hard drusen are small, circular structures with sharply defined borders and can occur either scattered apart or clustered together and both eyes; some even reside in the optic disc and are known as ‘optic disc drusen’ whereas soft drusen do not cause visual symptoms and thus do not need treatment.
Soft drusen are more likely to indicate late stages of disease and have softer edges than hard drusen, often appearing grouped or scattered across the retina. Not as prominent on an Amsler grid, soft drusen tend to show a pronounced ring of hyperautofluorescence on fluorescein angiography and do not require treatment, though eye health professionals will keep an eye out and offer lifestyle recommendations in order to prevent their conversion to hard drusen.
Treatment for Advanced AMD
Macular degeneration progresses when light-sensitive cells in your retina (macula) start to degenerate, leaving light-sensing cells without enough light sensing capabilities (which they use for reading and driving) deteriorate. While peripheral (side) vision remains functional, central vision loss makes reading or driving challenging and could eventually lead to blindness unless treated immediately with high dose vitamins and other supplements, as well as teaching how to monitor for changes. Eye professionals can slow its progress by treating symptoms early with high dose vitamins or supplements and teaching you ways of monitoring signs for changes.
Advanced AMD can be divided into two types, dry and wet. Wet AMD occurs when fluid accumulates beneath the retina, leading to abnormal blood vessel growth around the macula which then burst, leading to rapid vision loss. It accounts for 10% of cases of advanced macular degeneration.
The CATT study involved 1208 living participants at 44 clinical centers. Each visit involved a comprehensive dilated eye exam, refraction and VA measurements and imaging of the retina at baseline, before random assignment to ranibizumab or placebo injections over 24 months for monthly follow up evaluations – its primary goal being assessing anti-VEGF treatment’s impact on macular atrophy in both non-AMD (nAMD) and degenerative AMD eyes (dAMD).
For analysis purposes, this study was divided into three groups. The first consisted of 91 patients who started out without macular atrophy in both eyes at baseline. 47 individuals developed macular atrophy over time. Finally, 70 individuals received anti-VEGF injections in both eyes to assess how treatment affected asymmetry of macular atrophy progression rate; results demonstrated that treated eyes developed macular atrophy at significantly slower rates than untreated ones during year 1 follow-up.
Treatment for Macular Degeneration
Macular degeneration is a condition that primarily impacts your central vision, caused by damage to the macula in your retina – the area at the back of your eye that provides sharp central vision for reading, driving and threading needles – but symptoms include blurriness, dark areas and distortion in central vision.
Dry macular degeneration (DMD) is the initial stage of AMD, where light-sensing cells in your eye begin to degenerate over time, leading to blurry central vision and eventually loss altogether. There is no known cure for dry macular degeneration; however, maintaining a diet rich in fruits and vegetables as well as regular visits with your doctor may help slow its progress.
About 10% of people living with AMD also suffer from wet macular degeneration, in which abnormal blood vessels grow underneath the macula and cause bleeding and fluid leakage, potentially leading to rapid loss of vision if left untreated.
Wet AMD requires medication injected directly into the eye to reduce new blood vessel formation and stop fluid leakage from existing ones. Your doctor may also suggest laser surgery to treat any blood vessels that are leaking, as well as laser eye surgery to seal any leaky vessels in your eye.
Anti-VEGF medications are the cornerstone of treatment for wet macular degeneration, administered via eye injection to suppress chemicals in the body that trigger blood vessel development and growth. Popular options include bevacizumab, ranibizumab and pegaptanib.
Studies suggest that docosahexaenoic acid (DHA), an omega-3 very-long-chain polyunsaturated fatty acid, may provide protection from dry macular degeneration. More specifically, DHA appears to support production of elovanoids within retinal photoreceptor cells by stabilizing structure and function of these important cells; further research should confirm these findings.