Stem Cell Treatment for Macular Degeneration
Age-related macular degeneration (AMD) is an eye condition resulting in significant vision loss, but stem cells could offer hope to restore lost eye cells and provide vital trophic support to protect retinal cell survival.
Researchers have made major strides forward with cell replacement therapy for macular degeneration and other retinal diseases, using autologous stem cells as part of the therapy. In this article we’ll take a closer look at a variety of techniques.
Regenerative Medicine
Regenerative medicine utilizes the body’s own healing processes to heal diseased cells, tissues, and organs – with the goal of restoring function and improving quality of life for patients with macular degeneration and other ailments.
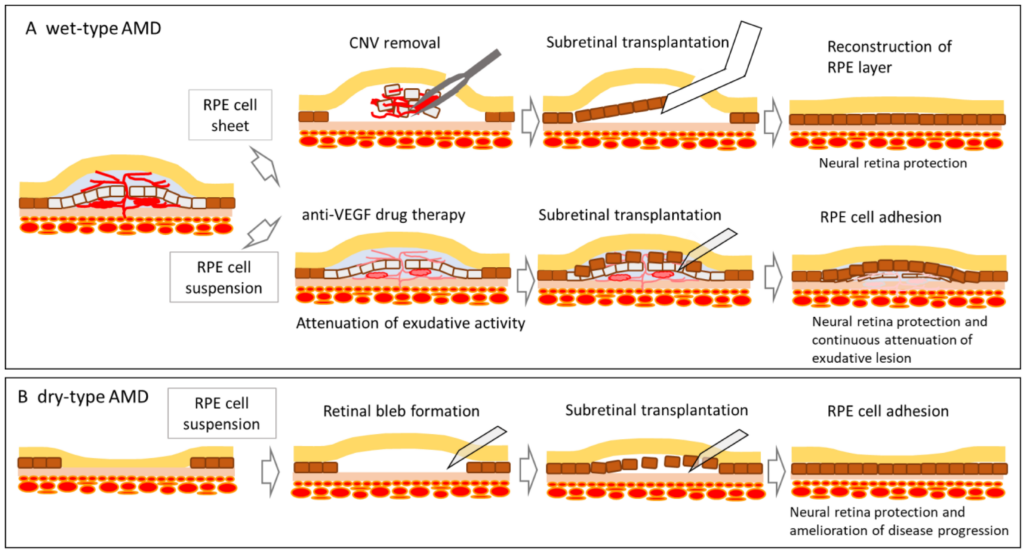
Stem cells may provide one approach for replacing retinal pigment epithelium (RPE) cells damaged by conditions like AMD. RPE is an epithelial layer behind photoreceptors which send visual signals directly to the brain. A pilot study demonstrated how RPE transplants restored vision in patients suffering from dry form AMD; additional trials are currently ongoing to examine whether this technique can also work against other forms of macular degeneration.
Stem cells possess the capacity to multiply and differentiate into various cell types, providing potential treatments for various health issues. Adult stem cells may even regenerate new tissues – making them an attractive candidate for regenerative medicine applications.
Regenerative medicine is an exciting area of research, where scientists explore how stem cells from our own bodies can be harnessed to repair damaged tissue and organs. Regenerative medicine has shown promise in treating various disorders such as heart disease, spinal cord injuries and arthritis.
Scientists are developing techniques to control the differentiation of stem cells into retinal pigment epithelium (RPE) cells for transplant into the eye. This research could significantly improve vision for those suffering from age-related macular degeneration or retinal diseases.
Macular degeneration stem cell treatments offer another innovative option in the form of induced pluripotent stem cells (iPSCs). These iPSCs, taken from your own blood and programmed to become any other cell type within your body, are grown into sheets one cell thick before implanted between RPE cells and photoreceptors to provide nutrition for these vital components of vision.
Animal models have demonstrated that using iPSCs for retinal regeneration to be successful; several clinics are offering human trials of this technology as well. Unfortunately, recent mishaps at a Florida clinic that injects patients’ eyes with their own RPE produced using their own iPSCs has raised concerns regarding its safety.
Autologous Stem Cells
Age-related macular degeneration can be devastating to vision. Even mild forms can limit central vision and eventually progress into legal blindness (unable to see Big E on eye chart; vision less than 20/200). New stem cell treatments show promise in restoring vision by either directly replacing lost retinal cells or secreting factors which promote survival of existing retinal cells.
Researchers are developing an innovative technique for treating macular degeneration using adult stem cells from patients’ own blood. These cells can then be transplanted back into the eye to replace damaged or degenerating retinal pigment epithelial (RPE) cells that contribute to AMD and vision loss, providing hope for those who have already lost their sight due to AMD. This reduces rejection risk while offering hope to those suffering late-stage AMD who may already be losing sight.
Multiple studies have demonstrated that human iPSC-derived RPE cells can restore visual function to mice with macular degeneration. These early results give scientists hope that this technology may provide a potential cure for humans with macular degeneration.
A clinical trial launched this year will use autologous RPE cells derived from autologous iPSC to treat people suffering from advanced dry macular degeneration, an early sign of wet macular degeneration. Through an approach similar to corneal transplantation, doctors will surgically implant into each eye a patch made up of cells made from one’s own cells, similar to how corneal transplantation replaces damaged corneal tissue with new ones made of ones own cells sourced from an autologous source such as RPE cells made from patient own cells or RPE cells harvested from another individual donor source if necessary.
These transplanted cells will nourish photoreceptors – retinal cells responsible for turning light into visual images – in hopes that this treatment can reverse symptoms associated with dry macular degeneration such as loss of central vision.
Health Canada recently hosted a one-day workshop to clear away any misconceptions or barriers to providing access to autologous cell therapy products that have been proven safe and effective. The workshop was co-sponsored by NYSCF-Robertson Stem Cell Prize, which supports research into regenerative medicine to bring treatments for macular degeneration and other conditions, and Canadian Institutes of Health Research.
Induced Pluripotent Stem Cells (iPSCs)
Researchers can turn skin or blood cells into stem cells by adding special genes. Once transformed, these stem cells can develop into any cell in the body – even macular degeneration! Researchers also use stem cells as models for disease and drug testing purposes.
Research with iPSCs seeks to develop new therapies for human disease by replacing damaged cells with healthy ones, similar to replacing retinal pigment epithelium (RPE) cells lost with age related macular degeneration, in order to restore vision.
Researching stem cell therapy involves transforming patient cells into induced pluripotent stem cells (iPSC), which have the capacity to become any cell in their bodies. Once formed, these iPSCs are directed toward becoming retinal pigment epithelium (RPE) cells to replace damaged RPE cells within animal models – leading to improved vision in many of them. Researchers hope to further refine and bring human clinical trials for this technology.
One challenge of using iPSCs for retinal regenerative medicine is ensuring the transplanted cells integrate smoothly into existing retinal tissue, so researchers are working hard to facilitate their incorporation through growth factors, special culture conditions, and genetic manipulation techniques.
Science Translational Medicine recently published a study using iPSC-derived RPE to restore blood-retinal barrier function in mice carrying mutations of genes associated with macular degeneration and aging. Mice receiving treatment demonstrated less degradation to their visual system and improved retinal pigmentation compared with untreated animals.
This research represents the first evidence that iPSCs can be used to prevent macular degeneration and other diseases of the retinal pigment epithelium (RPE). It represents an initial step in taking regenerative medicine out of the lab and into clinical settings. As this and other advances in stem cell treatments for macular degeneration continue, our role as ophthalmologists is expected to become increasingly vital, while patients requiring stem cell therapy will finally be able to receive it.
Bioengineered Implants
Researchers are exploring bioengineered implants as a potential treatment to restore vision in those suffering from retinal diseases such as dry age-related macular degeneration (AMD) and Retinitis Pigmentosa (RP). Both diseases cause the retina to deteriorate, leading to blurred or distorted central vision and impacting over 10 million Americans currently; their prevalence could reach as many as 196 million globally by 2020.
There is currently no cure for eye diseases that can lead to blindness, but studies have demonstrated the power of stem cells to slow their progress and potentially stop blindness from happening altogether. Scientists are working on methods for transplanting these stem cells that will regenerate damaged eye tissue; such treatments could include cells from under the retina referred to as the choroid layer.
These new treatments will involve using somatic cells from an adult patient as the source of induced pluripotent stem cells that will then be programmed into retinal pigment epithelial cells – cells found within the retina that provide support to photoreceptors to convert light to sight – as a source for macular degeneration replacement and also testing whether transplanted cells could restore sight for those suffering with RP and Stargardt disease.
Queen’s research has played a key role in creating cutting-edge healthcare technologies, including multifunctional biomaterials customized for specific medical interventions. These innovations have applications across fields like regenerative medicine, tissue engineering and 3D printing technologies.
Human embryonic stem cell (ES) transplants were recently found to help older mice suffering from macular degeneration regain some lost function, suggesting this therapy may offer hope to many patients suffering from macular degeneration and retinal diseases. The findings were published in Science Translational Medicine under Dr. Kashani who serves as director of NYSCF’s Regenerative Medicine program; funding came from National Institutes of Health grants.