What are the stages of diabetic retinopathy?
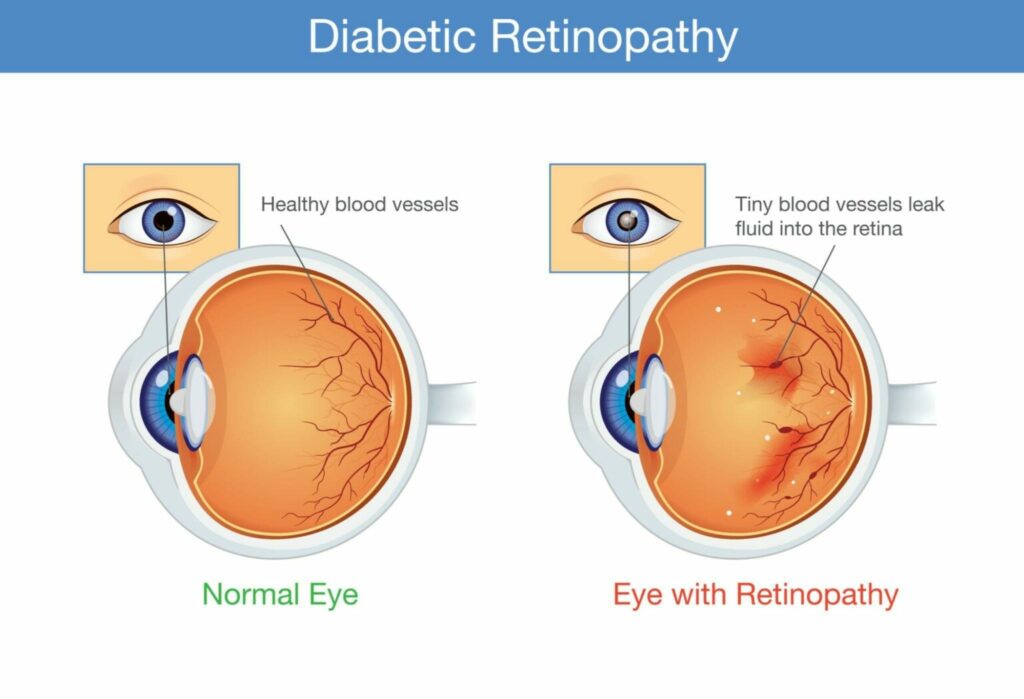
Diabetic retinopathy is a type of vision impairment that affects millions of people worldwide. It is a complication of diabetes that occurs when high blood sugar levels damage the blood vessels in the retina, which is part of the eye responsible for capturing and transmitting visual information to the brain. Over time, this damage can lead to vision loss or blindness.
There are several stages of diabetic retinopathy, each with different symptoms and levels of severity. It is important to understand these stages so that people with diabetes can take steps to prevent or slow down the progression of the disease.
Stage 1: Mild Nonproliferative Retinopathy
The first stage of diabetic retinopathy is mild nonproliferative retinopathy. During this stage, the blood vessels in the retina start to weaken and become damaged. This can cause small bulges or leaks to occur in the vessels, but the retina itself is not significantly affected.
At this stage, people with diabetic retinopathy may not experience any symptoms or vision problems. However, the damage to the blood vessels can still be seen during a comprehensive eye exam, which is why regular eye exams are important for people with diabetes.
Stage 2: Moderate Nonproliferative Retinopathy
The second stage of diabetic retinopathy is moderate nonproliferative retinopathy. During this stage, the damage to the blood vessels in the retina becomes more severe, and the vessels start to close off. This can cause a decrease in blood flow to the retina, which can lead to vision problems and vision loss.
People with moderate nonproliferative retinopathy may experience symptoms such as blurred vision, dark spots in their vision, and floaters. They may also notice that their eyesight is worse in the morning or after being active, and may feel eye strain or fatigue when performing tasks that require good vision.
Stage 3: Severe Nonproliferative Retinopathy
The third stage of diabetic retinopathy is severe nonproliferative retinopathy. During this stage, the damage to the blood vessels in the retina becomes even more severe, and many of the vessels are completely closed off. This can cause a significant decrease in blood flow to the retina, leading to vision problems and vision loss.
People with severe nonproliferative retinopathy may experience a variety of symptoms, including vision loss, floaters, and difficulty seeing in dim light. They may also experience a temporary loss of vision, called a “blackout,” as a result of decreased blood flow to the retina.
Stage 4: Proliferative Retinopathy
The fourth stage of diabetic retinopathy is proliferative retinopathy. During this stage, the retina begins to produce new blood vessels in an attempt to restore blood flow. However, these new blood vessels are abnormal and fragile, and can easily bleed into the eye. This can cause a number of serious complications, including vision loss, vitreous hemorrhage, and retinal detachment.
People with proliferative retinopathy may experience symptoms such as vision loss, floaters, and flashing lights. They may also experience a sudden decrease in vision as a result of blood entering the eye.
Stage 5: Advanced Proliferative Retinopathy
Advanced proliferative retinopathy is the final stage of diabetic retinopathy and is characterized by the growth of abnormal blood vessels in the retina and the vitreous, the clear gel that fills the eye. These blood vessels are weak and prone to leaking, causing significant damage to the retina and vision loss.
In this stage, the blood vessels can become so damaged that they can cause the retina to become detached, leading to vision loss. Additionally, scar tissue can form, causing the retina to shrink and pull away from the wall of the eye. This can result in retinal detachment and even total vision loss.
In advanced proliferative retinopathy, prompt treatment is necessary to prevent further damage to the retina and preserve vision. Treatment options may include laser therapy, which uses a high-energy beam of light to seal off leaking blood vessels, or surgery, such as a vitrectomy, which involves removing the vitreous gel and repairing the retina.
In some cases, the damaged blood vessels can cause a condition called neovascular glaucoma, where the growth of new blood vessels in the eye increases pressure, causing damage to the optic nerve and resulting in vision loss. This can be treated with medication, laser therapy, or surgery to remove the damaged blood vessels and reduce pressure.
It is important to monitor diabetic retinopathy closely and seek prompt treatment if necessary to prevent further damage to the retina and preserve vision. Regular eye exams and monitoring of blood glucose levels can help to detect the condition early and allow for prompt treatment.
Treatment of each stage of Diabetic Retinopathy
The treatment of diabetic retinopathy depends on the stage of the condition and the severity of the damage to the retina. In the early stages, the focus is on monitoring and controlling underlying diabetes to prevent further damage to the retina.
Treatment of Stage 1: Mild Non-Proliferative Retinopathy
In this stage, the goal is to prevent the progression of the condition to more severe stages. This can be achieved by controlling blood glucose levels and blood pressure, quitting smoking, and getting regular eye exams. In some cases, laser therapy may be used to seal off leaking blood vessels, but this is usually not necessary in the early stages.
Treatment of Stage 2: Moderate Non-Proliferative Retinopathy
In this stage, the focus is on preventing the progression of the condition to more severe stages and preserving vision. This can be achieved by controlling blood glucose levels and blood pressure, quitting smoking, and getting regular eye exams. In some cases, laser therapy may be used to seal off leaking blood vessels, which can help to prevent further damage to the retina.
Treatment of Stage 3: Severe Non-Proliferative Retinopathy
In this stage, the goal is to prevent the growth of new, weaker blood vessels and preserve vision. This can be achieved through laser therapy, which seals off leaking blood vessels and reduces the risk of further damage to the retina. In some cases, surgery may be necessary to repair the retina and prevent retinal detachment.
Treatment of Stage 4: Pre-Proliferative Retinopathy
In this stage, the focus is on preventing the growth of new blood vessels and preserving vision. Laser therapy is often used to prevent the progression of the condition and reduce the risk of vision loss. In some cases, anti-VEGF injections may be necessary to prevent the growth of new blood vessels, which can cause significant damage to the retina.
Treatment of Stage 5: Advanced Proliferative Retinopathy
In this stage, prompt treatment is necessary to prevent further damage to the retina and preserve vision. Laser therapy and surgery may be used to repair the retina and prevent retinal detachment. In some cases, anti-VEGF injections may be necessary to prevent the growth of new blood vessels and reduce the risk of vision loss. In some cases, the damaged blood vessels can cause neovascular glaucoma, which can be treated with medication, laser therapy, or surgery.
Treatment with Injections
Anti-VEGF (vascular endothelial growth factor) injections are a type of treatment used for diabetic retinopathy, especially in its later stages. VEGF is a protein that promotes the growth of new blood vessels, which can cause significant damage to the retina in diabetic retinopathy. Anti-VEGF injections work by blocking the effects of VEGF and preventing the growth of new blood vessels, reducing the risk of vision loss.
The injections are typically given directly into the eye and are performed in a doctor’s office or clinic. The number of injections required depends on the severity of the diabetic retinopathy and the response to treatment. In some cases, several injections may be necessary to control the growth of new blood vessels and preserve vision.
The benefits of anti-VEGF injections for diabetic retinopathy include reduced risk of vision loss, improved vision, and improved quality of life. However, there are also potential risks and side effects associated with the treatment, including eye pain, swelling, and vision changes. In some cases, the injections may also increase the risk of eye infections or lead to an increased need for glasses or contacts.
It is important to discuss the benefits and risks of anti-VEGF injections with your doctor and to carefully monitor your vision and eye health after the injections. Regular eye exams and monitoring of blood glucose levels can help to detect any changes in your diabetic retinopathy and allow for prompt treatment.
Anti-VEGF injections are a type of treatment used for diabetic retinopathy, especially in its later stages. The injections work by blocking the effects of VEGF and preventing the growth of new blood vessels, reducing the risk of vision loss. The benefits of anti-VEGF injections include reduced risk of vision loss and improved vision, but there are also potential risks and side effects associated with the treatment. It is important to discuss the benefits and risks of anti-VEGF injections with your doctor and to closely monitor your eye health after the injections.
Treatment with Laser Surgery
Laser surgery, also known as photocoagulation, is a common treatment for diabetic retinopathy, especially in its early and intermediate stages. The goal of laser surgery is to prevent the progression of diabetic retinopathy and preserve vision by sealing off leaking blood vessels and reducing the risk of further damage to the retina.
The laser surgery is performed in a doctor’s office or clinic and typically takes about 30 minutes to an hour. A local anesthetic is used to numb the eye, and a special device is used to deliver the laser energy to the affected areas of the retina. The laser energy seals off leaking blood vessels and reduces the risk of further damage to the retina.
The benefits of laser surgery for diabetic retinopathy include reduced risk of vision loss, improved vision, and improved quality of life. However, there are also potential risks and side effects associated with the treatment, including eye pain, swelling, and vision changes. In some cases, laser surgery may also increase the risk of eye infections or lead to an increased need for glasses or contacts.
It is important to discuss the benefits and risks of laser surgery with your doctor and to carefully monitor your vision and eye health after the surgery. Regular eye exams and monitoring of blood glucose levels can help to detect any changes in your diabetic retinopathy and allow for prompt treatment.
Laser surgery is a common treatment for diabetic retinopathy, especially in its early and intermediate stages. The goal of the surgery is to prevent the progression of diabetic retinopathy and preserve vision by sealing off leaking blood vessels and reducing the risk of further damage to the retina. The benefits of laser surgery include reduced risk of vision loss and improved vision, but there are also potential risks and side effects associated with the treatment. It is important to discuss the benefits and risks of laser surgery with your doctor and to closely monitor your eye health after the surgery.
Treatment with Vitrectomy
If you have advanced diabetic retinopathy, a vitrectomy may be necessary. The vitreous, jelly-like fluid in the center of the eye and retinal issues are both treated with this eye surgery. The operation can remove scar tissue, blood, or fluid, and some vitreous gel to allow light to properly concentrate on the retina. Retinal detachments may be treated concurrently.
In conclusion, the treatment of diabetic retinopathy depends on the stage of the condition and the severity of the damage to the retina. In the early stages, the focus is on controlling underlying diabetes and preserving vision. In later stages, laser therapy, surgery, and medications may be necessary to prevent further damage to the retina and preserve vision. Diabetic retinopathy is a progressive condition that affects the blood vessels in the retina, leading to vision loss and blindness. The final stage, advanced proliferative retinopathy, is characterized by significant damage to the retina and the growth of abnormal blood vessels. Prompt treatment is necessary to prevent further damage to the retina and preserve vision. Regular eye exams and control of blood glucose levels are important for the early detection and management of diabetic retinopathy.
FAQs for Stages of Diabetic Retinopathy
What is the diabetic retinopathy 4 2 1 rule?
By applying the “4-2-1 rule,” it is diagnosed. If the patient has any of the following: venous beading in two or more quadrants, diffuse intraretinal hemorrhages, or microaneurysms in one or more quadrants, a diagnosis is determined.
What is the rate of development of diabetic retinopathy?
Diabetes’ consequence, diabetic retinopathy, is brought on by high blood sugar levels harming the retina (retina). If undetected and mistreated, it can result in blindness. However, it often takes a number of years for diabetic retinopathy to progress to the point where it can endanger your vision.
Why does diabetic retinopathy get worse?
When a patient with diabetes begins receiving effective therapy for hyperglycemia, their diabetic retinopathy (DR) tends to get worse. It appears before the long-term advantages of enhancing glycemic control and has been linked to risk factors such as poor blood glucose control and hypertension.