In the arena of health, knowledge is key. Today, we take on one of the most important yet often neglected areas of health, pre-diabetes eye problems. First, we need to understand what is pre-diabetes before we can delve into what, if any, eye problems are associated with it and how to prevent and treat them.
Pre-diabetes is a condition when your blood glucose levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. Alerting you to this warning light can give you a chance to make changes to stop the progression of Type 2 diabetes. So what do you think happens to your eyes?
Pre diabetes and eye problems
There are a multitude of aspects that may account for the correlation between pre-diabetes and several eye problems that can arise. The spiked blood sugars in pre-diabetes could damage the small blood vessels in the eyes, resulting in many complications. By understanding the correlation with pre-diabetes, people can protect themselves by getting tests and treating their eyes before it gets worse.
The different conditions of the eyes that pre-diabetic people are at higher risk of are ‘diabetic retinopathy’ this is when the blood vessels in the back of the eye are damaged and could lead to sight damage if not treated. Glaucoma is where the eye is put under constant pressure (from the inside pushing out which is called IOP) and has a detrimental on effect the optic nerves in the eye. The most common condition that pre-diabetic people are diagnosed with is cataracts.
Both type 1 and type 2 diabetes can contribute to glaucoma and cataracts. It’s important to know how diabetes affects your eyes in these diseases. The effects may help in treating and managing glaucoma and cataracts. We will discuss how diabetes contributes to glaucoma and cataracts next!
Glaucoma
A group of eye conditions characterized by damage to the optic nerve often, but not always, associated with increased intraocular pressure (IOP).
Elevated IOP is caused by a build-up of fluid in the eye and can eventually cause damage to the optic nerve.
Elevated Intraocular Pressure (IOP)
The eye normally has a built-in control system that allows fluid to be drained out of the eye at the same rate that it is produced. This keeps pressure in the eye relatively stable. However, diabetes can interfere with this system, causing the outflow of fluid from the eye to decrease. As fluid continues to be produced in the eye, a build-up of fluid and an increase in eye pressure occurs. Over time, elevated eye pressure can damage the optic nerve, leading to glaucoma.
Blood Vessel Changes
One of the diseases, diabetes, can also impact the vessels within the body. Damage to the small blood vessels found all over the body and also in the eye is directly related to diabetes. These changes within the blood vessels are linked to the supply of blood flow to the optic nerve which is associated with the damaged nerves found in glaucoma.
It is interesting to note that many things affect the body slightly differently than you would think they would. For example, our notes state that neuropathy and retinal blood pressure increase with the causes of damage in the body. The notes also let us know that inflammation and oxidative stress are also causes and have an effect on the body of a diabetic. But when you stop and think about it for a moment what all comes along with chronic inflammations? Yes, several things like being sick easily or the body trying to fight off bacteria or many other infections but really Overall, oxidative stresses and inflammation play a critical role in the pathogenesis of diabetes and its secondary complications, such as retinopathy, nephropathy, cardiovascular diseases, and an impaired wound healing. We need to look also into the fact that inflammation and retinal oxidative stress have been implicated in the pathogenesis of both ischemic and non-ischemic retinopathies (Chatterjee and Seasholtz, 2011). Going off of that we could say that it is possible that inflammation and oxidative stress could play a role in glaucoma as well. Yes, these symptoms and diseases are commonly seen in the body of a diabetic but can we not relate them to a glaucoma patient?
Neurodegeneration
Diabetes also contributes to and accelerates the neurodegenerative processes related to the optic nerve. These neurodegenerative changes can over time worsen optic nerve function in glaucoma.
Cataracts
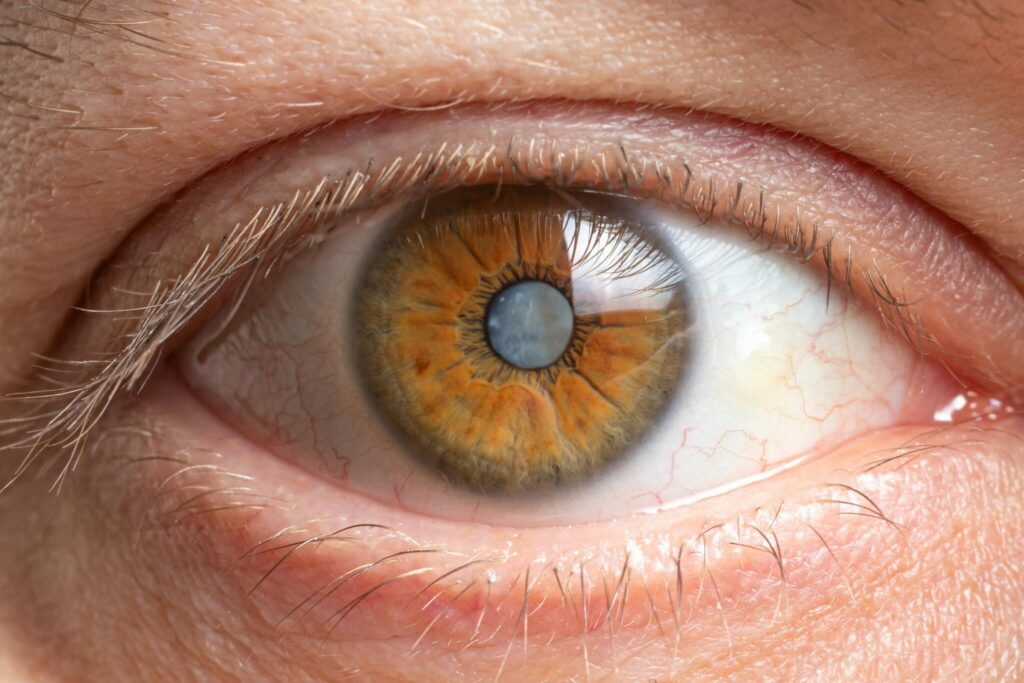
When people have cataracts the lens of their eye becomes cloudy. This makes it so the light is unable to pass through the eye resulting in a loss of eyesight. There are different types of cataracts many of which can develop through diabetes as a cause. Everyone takes in light through the iris and the cornea. The eyes have a lens that is surrounded by a capsule and the purpose of the lens is to focus many of the light rays that come into the eye onto the retina.
Increased blood sugar levels from diabetes can cause the lens proteins to become glycated which in turn can make proteins cloudy and lens opacities are also a factor for diabetic cataracts.
Osmotic Changes
As blood sugar levels change, this can create a change in osmotic pressure inside the lens which can then change the transparency of the lens and affect cataract formation.
Decreased Regenerative Capacity
Diabetes is believed to damage the normal repair process that helps heal even minor damage to the lens. The impaired ability of the lens to regenerate used protein may help proteins clump together and settle.
Calcium Build-up
The lens depends completely upon the free movement of fluids in the eye to supply the fiber cells with essential nutrients. If the osmolarity of the lens is upset so is essential fluid movement, leaving the lens fiber cells without proper nutrition. The imbalance of osmolarity can come from such means as high blood glucose, sorbitol concentration, low ascorbic acid, or reduced power.
Nuclear Lens Changes Anti-BRD, or senile cataract, is the term used to describe cataracts caused by old age. It is known that the older a person is, the greater the chances of developing nuclear lens changes. However, in a person with diabetes, the odds of developing cataracts are estimated to be 60% more likely than a person without diabetes.
Reduced antioxidant defense This could be problematic because having an antioxidant defense system helps protect the lens from being damaged by the many chemical reactions occurring within the lens every day. Whenever the lens metabolizes glucose, such as occurs in people with diabetes, it uses up abundant amounts of ascorbate in oxidative reactions. Besides ascorbate, there are many other potential antioxidants that have been found in the lens. Since ascorbate is very hydrophilic, it may also function as a membrane antioxidant (Bursell and Clermont). If it was not for this so-called defense mechanism found in the human lens, there would not be anything to stop the free radicals from stripping the lens of all its proteins and thus no longer be transparent.
Free radicals can damage proteins by oxidizing important amino acids such as histidine, lysine, and threonine. Subsequently, the proteins tend to develop different types of bond cross-links that influence irreversible denaturation and compromise the very low protein turnover in the lens, which is needed to maintain its optical clarity. To overcome this, cellular systems down-regulate the synthesis of specific proteins, repair damaged proteins, and identify abnormal proteins for degradation.
One factor in the lens’ elevation of sugar levels is the altered sorbitol pathway. Glucose is converted to sorbitol, presumably in the neural retina, and then sorbitol is metabolized to fructose. When glucose levels in the eye are elevated, more glucose enters the lens than is normally metabolized. Since the enzyme used to convert sorbitol to fructose is not present in the lens, sorbitol will accumulate within the lens, and its subsequent oxidation to fructose will pull in water, causing osmotic changes and lens swelling.
In summary, diabetes produces the contribution and the progression of two glaucoma and cataracts using different mechanisms, such as changes in intraocular pressure rate, vascular alterations, oxidative stress, neurodegeneration, glycation of the lens, etc—, osmotic changes, and sorbitol pathway alterations. The importance of right eye interventions for diabetes could be able to improve blood glucose levels and then the sight-threatening complications.
Symptoms and Indicators of Pre-Diabetic Eye Problems
Prompt detection is crucial to limiting the impact of eye issues triggered by pre-diabetes. Warning signs include:
- Blurred sight
- Inconsistent sight
- Nighttime visual challenges
- Specks or dark strings that venture into the field of sight
- Eye pain or pressure
Diagnosing Eye Problems Caused by Pre-Diabetes
Necessary eye checks are vital to promptly discovering even pre-diabetes-based eye issues. With many diagnostic implements at their disposal, eye care professionals embrace dilated eye checks, visual acuity checks, and tonometry to judge the quality of the eye’s health and to perceive deviations that suggest a problem developing.
Preventing Eye Problems Caused by Pre-Diabetes
Prevention stands paramount if healthy sight is to be enjoyed without let up despite pre-diabetes. Prevention bears on several behaviors:
- Proper nutrition, thanks to eating many fruits and vegetables, and whole grains
- Ongoing, substantial physical movement
- Meticulous monitoring of blood sugar levels
- Keeping off tobacco
- Battling other health woes like high cholesterol, and high blood pressure.
Pre-diabetes is when your blood sugar level is higher than it should be but not high enough to be called full-blown diabetes. It is extremely important to manage your pre-diabetes if you do not want to lose your eyesight.
There are many things that can be done to help manage your pre-diabetes. The first thing you should do when you are diagnosed with pre-diabetes is make a plan with your healthcare provider. The next thing you should do is follow the plan that you have made with your healthcare provider. The plan will include what you should eat if you should be taking any medications, what you should do for physical activity, and any smoking or drinking.
Another thing that you should do to manage your pre-diabetes is take your medications if you have been put on some. If you are worried about having to stick yourself with a needle all of the time, there are other medication options that you could do as well without having to stick yourself with a needle. You should also take your medications at the same time each and every day.
Another strategy you should use when trying to manage your pre-diabetes is to stick yourself with a needle to test and see what your blood sugars are. You should not only test your blood sugar once a day, you should test your blood sugar multiple times a day. You should also try to make sure that you are testing your blood sugar around the same time every day.
The next strategy you should use is to stress less. Some ways that you can do to stress less is, to let go of things that are out of your control, do breathing exercises, and go for walks. If all else fails, call a friend and talk it out. The last strategy you should use is to seek the support of a healthcare professional or diabetes educator.
What are the Treatment Options?
The treatment options for pre-diabetes eye problems differ depending on the pre-diabetes condition that you are afflicted with. The treatment options available include:
- Intravitreal injections – this type of treatment is for pre-diabetes-related diabetic retinopathy.
- Laser treatment – is probably the most common treatment method for pre-diabetes eye complications as it is effective. This method of treatment is often used if the leaking blood vessels appear in the eyes from the high blood sugar levels.
- Surgery – if the cataracts in the eyes become advanced patients could possibly go in for surgery or the same goes for when glaucoma appears.
Lifestyle Changes for Better Eye Health with Prediabetes
Aside from any medical interventions, there are changes in lifestyle that can be made to help with eye health with prediabetes and these include:
- Eating healthy which is a low sugar/low saturated fat diet
- Exercise
- Proper rest
- Proper eye care using no screen, constant blinking, and breaks.
Overall, the eyes can be affected by the body’s pre-diabetes consequences because if our normal blood sugar levels are above the normal glucose, the blood vessels/retina are affected and you won’t be able to see. Also, the retina could lose normal vision causing it to become a blurry brown mess. The person who has pre-diabetes and his family should be notified of the same to find the necessary course of weight management, exercise, and diet control to bring down the symptoms of the body’s pre-diabetes consequences.
Pre-diabetes can sometimes be reversed with lifestyle changes including losing a modest amount of weight if you are overweight, eating healthful foods, and being physically active for at least 150 minutes per week.
FAQ’s
If I have prediabetes, how often should I have my eyes checked?
An individual with prediabetes is advised to have a comprehensive eye exam annually.
Are there dietary supplements that an individual could take to minimize their risk of developing pre-diabetes in the eye?
There are no particular supplements that would benefit the eyes.
An overall healthy, well-balanced diet, that includes all the vitamins and minerals necessary for the body to function properly will help in the long run to keep the eyes healthy. A diet that is low in fats and sugar and high in fiber, as well as colorful fruits, vegetables / dark leafy green vegetables, and Omega-3 fatty acids as found in cold-water fish such as salmon and flax seeds can help maintain eye health.
Will a pre-diabetes eye problem always lead to blindness?
If left unattended, pre-diabetes eye problems specifically diabetic retinopathy can maybe destroy eyesight to some extent. However, if one gets a quick intervention the problem subsides thus significantly reducing the risk of blindness.
What should I do if I notice sudden changes in my vision?
You need to receive immediate medical attention if you experience any kind of sudden changes to your vision. Call your eye doctor or healthcare provider for a complete exam and guidance.