When you notice changes in your vision, it’s natural to feel concerned. Many people wonder about the connection between eye floaters and macular degeneration. I’m here to give you clear, simple answers based on my years of clinical experience.
The differences between floaters and macular degeneration is significant. They affect separate parts of the eye and are not directly related. One does not cause the other. It’s easy to confuse them because both conditions can appear as we get older, but the difference between floaters and macular degeneration becomes clear when you compare how each affects vision. However, the spots they cause look and act differently.
Age plays a major role in macular degeneration. The risk of AMD rises sharply as we grow older, and among people 85 years and above, about 46.6% are affected.
In this article, I will walk you through what each condition is, what the symptoms are, and when you should talk to your doctor. My goal is to give you the information you need to understand your eye health with confidence.
KEY TAKEAWAY
- Eye floaters do NOT cause macular degeneration.
- Macular degeneration does NOT typically cause floaters.
- They affect different parts of the eye.
- Both are common age-related changes.
- Each requires different treatment approaches.
Understanding Eye Floaters
Many patients come to me worried about seeing little specks or lines floating in their vision. Most of the time, these are simply eye floaters, which are very common and usually harmless. Let’s break down what they are and why they happen. A recent patient said” I have a donut shaped blurred spot in my straight ahead vision.”
What Are Eye Floaters?
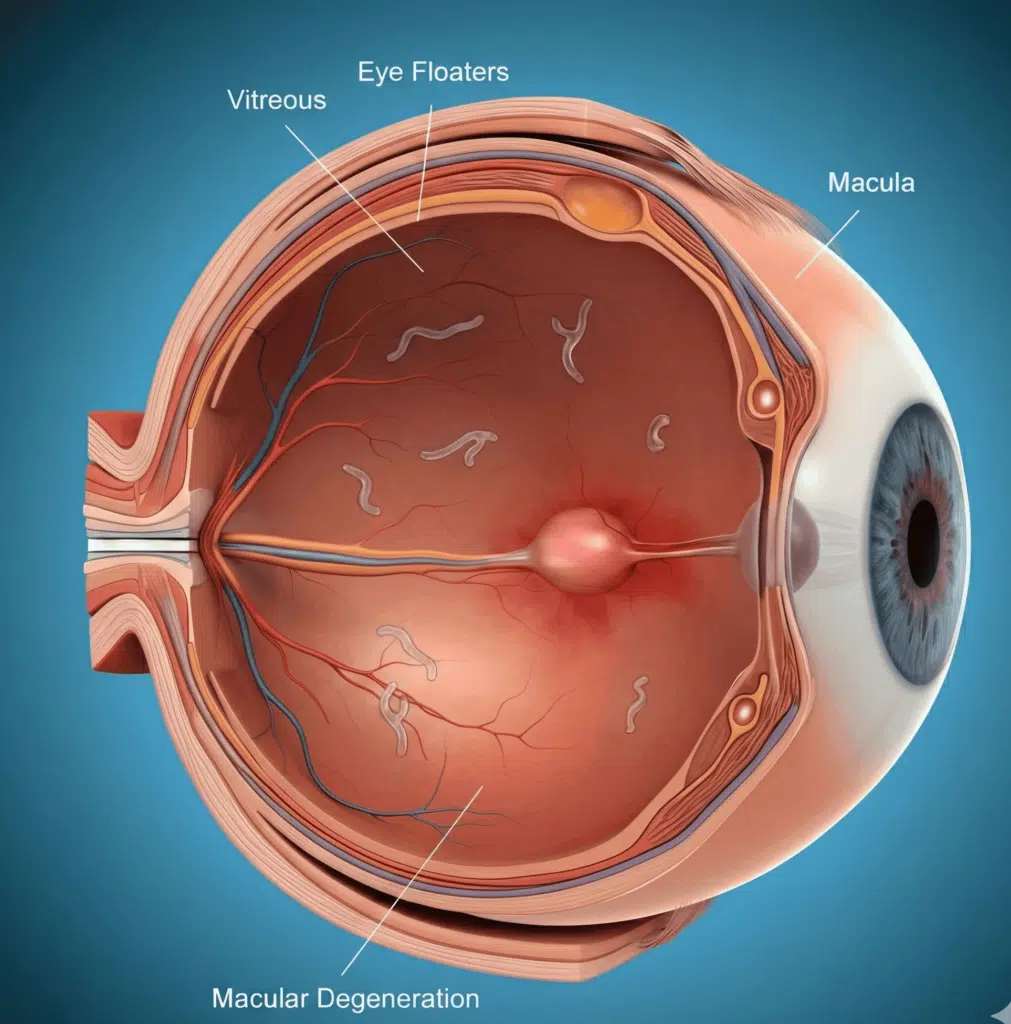
Eye floaters are small, squiggly shapes in your vision. Some look like cobwebs. They are usually harmless and mostly related to aging changes in the gel of the eye.
You may notice:
- Tiny black dots, specks, strands, or cobweb-like shapes
- More visible against bright backgrounds (white wall, computer screen, clear sky)
- They move when your eye moves, and when you try to look at them directly, they seem to shift away
- They tend to be in the same spot most of the time.
Why this happens:
- The inside of your eye is filled with a gel called the vitreous
- With age, this gel becomes less firm and forms tiny clumps
- These clumps cast shadows on the retina, and you see them as floaters
What Causes Eye Floaters?
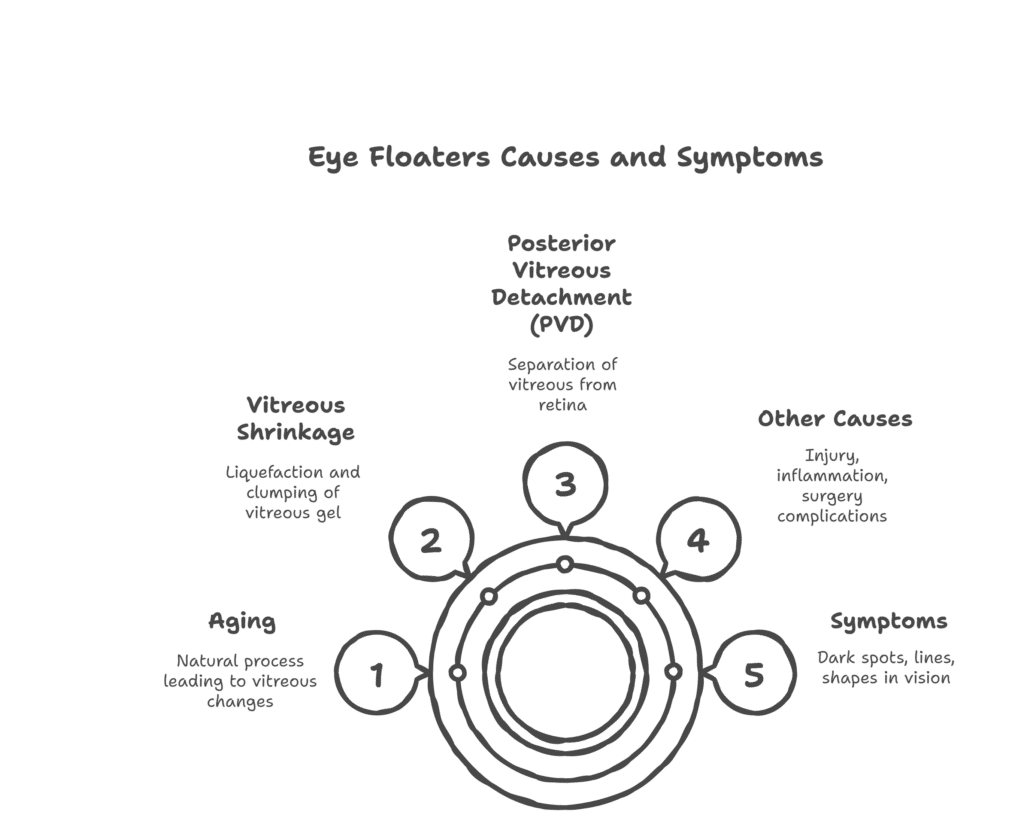
The most common cause of eye disorder floaters is natural aging. As you get older, the vitreous gel inside the eye becomes more liquid and starts to shrink, forming tiny clumps.
What happens with age:
- The vitreous gel slowly shrinks and becomes less firm
- It may pull away from the retina, known as a posterior vitreous detachment (PVD)
- A PVD is usually normal and not an emergency
- Around 75% of people develop PVD by age 65
- This usually leaves a large floater right in front of the macula and can be very annoying.
Other causes of floaters may include:
- Eye injury or trauma
- Inflammation inside the eye (uveitis)
- Complications after eye surgery
- Higher risk in people who are very nearsighted or have diabetes
In most cases, floaters are simply a natural part of aging, even though they are considered an eye disorder symptom.
Symptoms of Eye Floaters
The experience of having eye floaters is a bit different for everyone, but here are the most common symptoms:
- Seeing small dark spots, squiggly lines, or shapes like rings or cobwebs.
- The shapes move when you move your eyes and seem to drift when your eyes are still.
- They are easier to see against a plain, bright background.
- They may be annoying, but they do not cause pain.
Most people get used to their floaters over time, and the brain learns to ignore them.
Understanding Macular Degeneration
Now, let’s talk about a different condition called age-related macular degeneration, or AMD. When understanding what macular degeneration is, it’s important to know it is one of the leading causes of vision loss in adults over 50. Unlike floaters, macular degeneration affects the central vision, which you use to see things straight ahead.
What is Macular Degeneration?
Macular degeneration is an eye disorder; floaters are not a symptom of it. It affects a tiny part of your retina called the macula. The macula is responsible for your sharp, detailed central vision. You need it for tasks like reading, driving, and recognizing faces. Ruth, a patient said “ I first noticed that door frames looked curved and lines in books and papers were distorted and some were missing letters.”
While floaters are in the vitreous gel in the middle of your eye, macular degeneration damages the light-sensing cells in the retinal tissue at the very back of your eye.
This condition usually gets worse over time. It doesn’t cause complete blindness because it doesn’t affect your peripheral, or side, vision. However, it can make it very difficult to perform daily activities. Understanding what macular degeneration is is the first step in managing it.
Types of Macular Degeneration
There are two main types of AMD: dry and wet.
1. Dry AMD: This is the more common form, making up about 90% of all cases. It happens when the cells of the macula break down slowly over time. Yellow deposits called drusen build up under the retina. Vision loss from dry AMD is gradual and often less severe than the wet form. However, dry AMD can sometimes turn into wet AMD.
2. Wet AMD: This form is less common but much more serious. It occurs when abnormal blood vessels grow underneath the macula. These vessels are fragile and can leak blood and fluid, which damages the macula quickly. Vision loss from wet AMD can happen rapidly, sometimes in just days or weeks, and requires urgent medical treatment. Mike L said “ I woke up one day and I couldn’t see faces clearly with my right eye”
Symptoms of Macular Degeneration
Macular degeneration symptoms are very different from floater symptoms because they affect central vision rather than moving across the field of view.
Central Vision Changes:
- Blurred or distorted central vision: You might find that the center of your vision is fuzzy.
- Straight lines look wavy: This is a key sign called metamorphopsia. For example, a door frame or telephone pole might look bent.
- A dark or empty spot: You might notice a blind spot in the center of your vision, known as a scotoma.
- Trouble recognizing faces: Faces might appear blurry.
Functional Impact:
- Trouble reading, even with glasses: Reading small print or lengthy texts can become challenging, requiring additional effort or magnification tools.
- Problems driving, especially at night: Nighttime driving may feel unsafe due to reduced clarity, glare from oncoming headlights, or difficulty gauging distances.
- Difficulty seeing in low light: Dimly lit environments, such as restaurants or theaters, may make it harder to see details or move around confidently.
- Need for brighter light for tasks: Everyday tasks like sewing, reading, or cooking may require stronger light to see clearly, as vision under normal lighting feels insufficient.
- Colors appear less vivid: Colors may look duller or washed out, making it harder to distinguish between similar shades or notice subtle details.
Unique to Wet AMD
- Sudden vision changes: Wet AMD can cause abrupt alterations in vision, such as blurry or distorted sight, which may develop rapidly over just a few days.
- Rapid progression: Unlike dry AMD, the wet form can advance quickly, leading to significant vision loss in a short period of time if left untreated.
- Objects appear smaller (micropsia): Affected individuals might notice that objects seem smaller than they truly are, which can further disrupt perception and make everyday tasks more challenging.
- The only good thing, if you can call it that about wet AMD is that there are more treatment options than the dry version of floaters.
Unlike floaters that drift across your vision, macular degeneration symptoms stay fixed in the central line of sight and do not move.
The Key Differences: A Side-by-Side Look
To make it easier to see the difference between floaters and macular degeneration, let’s compare them directly.
| Feature | Eye Floaters | Macular Degeneration |
| Location in the Eye | Vitreous humor (the gel in the middle of the eye) | Macula (the central part of the retina at the back of the eye) |
| What’s Affected | The gel-like fluid inside the eye | The light-sensing tissue of the macula |
| Type of Vision Change | Spots or shadows that move across your entire field of vision | A stable blur, distortion, or dark spot in your central vision |
| Movement | They drift and float when you move your eyes | The spot or blur stays in the center of your vision and does not move |
| Onset | Often gradual, but can appear suddenly with a PVD | Gradual (dry AMD); can be sudden and rapid (wet AMD) |
| Typical Age | Common at any age, but most frequent from 50 to 75 | Usually starts after age 50 |
| Progression | Usually stable and don’t get worse after they appear | A progressive condition that worsens over time |
| Treatment | Rarely needed; usually just observation | AREDS2 vitamins (dry), injections, or laser (wet) |
| Causes Blindness | No, they do not cause blindness | It can cause loss of central vision, but not total blindness |
| Relationship | No direct link. Floaters do not cause AMD. | No direct link. AMD does not cause floaters. |
As you can see, these two conditions are fundamentally different. Think of eye floaters like clouds floating in front of a camera lens, which can be annoying but don’t damage the camera. Macular degeneration is more like damage to the camera’s sensor itself or the film, which affects the quality of the picture. The key takeaway is that eye floaters do not cause macular degeneration. You can have both floaters and AMD, and most likely at least have some floaters if you are over the age of 30. AMD doesn’t usually show up until about 65 on average.
Why do people confuse these conditions?
It is completely understandable to worry when you notice any changes in your vision. Your eyesight is precious, and hearing medical terms can be alarming. The main reasons people confuse these conditions are:
- Both are age-related: They both become more common as we get older, especially after age 50.
- Both affect vision: They both cause visual disturbances that can be concerning.
- Both can involve “spots”: This is a big point of confusion. However, the spots from floaters are defined shapes that drift around, while the spots from macular degeneration are blurry, distorted, or dark areas that are fixed in your central vision. One patient asked “why does the spot in my good eye move and the dark spot in my bad eye stay in the middle?” I answered “because one is a floater (the good eye) and the other is due to the AMD.”
- They can happen at the same time: Since both are common with age, it’s possible for a person to have both eye floaters and macular degeneration at the same time, but one does not cause the other.
When to see an Eye Doctor?
Knowing when to seek medical help is crucial for protecting your vision. Some symptoms require immediate attention, while others can be discussed at a regular appointment.
Emergency Symptoms: See a Doctor Immediately for Floaters
- Sudden Appearance of Many New Floaters
If you notice a sudden increase in the number of floaters in your vision, it could be a sign of a serious problem that requires prompt medical attention.
- Floaters Accompanied by Flashes of Light
The combination of floaters and flashes of light can indicate changes in the retina, which may lead to more severe complications if not treated quickly.
- A Dark Curtain or Shadow Over Your Vision
The presence of a dark shadow or curtain moving across your field of vision is often linked to retinal detachment, a condition that needs immediate intervention.
Experiencing sudden or significant loss of vision is always a serious concern, as it may be a symptom of an ocular emergency such as retinal detachment or other critical issues.
These symptoms may warn of retinal detachment, which is a medical emergency. If any of these occur, contacting an eye doctor or seeking emergency care without delay is essential to protect your vision.
- Sudden Onset of Distorted Vision
If you suddenly notice distortion in your vision, such as straight lines appearing wavy or bent, it could be an early sign of advanced macular degeneration. This symptom should not be ignored and requires immediate attention from an eye care professional.
- Rapid Increase in Central Vision Blur
A rapid or noticeable decline in the clarity of your central vision may indicate the development of wet age-related macular degeneration (AMD). Prompt evaluation is crucial to determine the cause and begin appropriate treatment.
- Sudden Appearance of Dark Spot in Central Vision
The sudden presence of a dark or blank spot in your central field of vision can be an alarming symptom. This often signifies macular damage and calls for urgent assessment to prevent further vision loss.
- Dramatic Change in How Straight Lines Look
If straight lines suddenly seem curvy, broken, or uneven, it could be a sign of fluid leakage or abnormal blood vessel growth in the retina hallmark of wet AMD. Quick intervention by an eye specialist is essential in such cases.
These symptoms may point to wet AMD, a condition requiring urgent medical attention and treatment to preserve as much vision as possible. Early detection and timely care can make all the difference in managing this serious eye condition effectively.
Schedule a Regular Appointment
Non-Urgent but Important Signs
- Gradual increase in floaters
Seeing more floaters over time might indicate changes in your eye’s vitreous gel or retina. While floaters are common with aging, a noticeable increase should be discussed with an eye doctor. - Slow changes in vision clarity
If your vision gradually becomes blurry or less sharp, it could be a sign of underlying eye conditions, including early AMD or cataracts. - New difficulty with reading or recognizing faces
Struggling to read small print or identify familiar faces might suggest a minor but important change in central vision that requires evaluation. - Trouble adapting to light changes
Finding it harder to adjust between bright and dim environments can signal early retinal or macular issues. - Any new or changing vision symptoms
Regardless of how minor a symptom may seem, any unexplained or persistent changes in vision warrant a conversation with your eye care provider.
Preventive Care
- Annual eye exams for adults 50+
Routine comprehensive eye exams are crucial for catching conditions like AMD in their early stages, especially as you age. - Bi-annual exams if family history of AMD
If you have a family history of macular degeneration, more frequent screenings can help monitor and detect potential issues sooner. - Amsler grid monitoring at home
Using an Amsler grid regularly can help you quickly identify any distortions or changes in your central vision. Place the grid in a well-lit area and check one eye at a time, focusing on the center dot. Any wavy, broken lines or dark spots should be reported to your doctor. - Immediately check if there are any concerns.
If you notice anything unusual about your vision, don’t wait; schedule an appointment as soon as possible. Early action ensures the best outcomes for your eye health.
How Eye Floaters Are Diagnosed?
- Dilated Eye Examination
Your doctor will perform a thorough dilated eye examination to assess the health of the retina and detect any abnormalities. - Visual Field Testing
This helps evaluate the impact of floaters on your peripheral vision and overall visual field. - Evaluation to Rule Out Retinal Tears/Detachment
Floaters can sometimes signal more serious issues, such as retinal tears or detachment, which require immediate attention. - Usually, No Special Imaging is Needed for Common Floaters
For typical floaters, additional imaging tests are generally unnecessary. - OCT Scan if Underlying Condition Suspected
If your doctor suspects an associated condition, Optical Coherence Tomography (OCT) may be used to obtain detailed images of the retina.
How is Macular Degeneration Diagnosed?
- Comprehensive Eye Exam with Dilation
Your doctor will perform a complete eye exam, including dilation, to examine the retina and macula closely. - Amsler Grid Test
This simple test checks for distortions or missing areas in your central vision, helping to detect early signs of macular degeneration. - Optical Coherence Tomography (OCT)
This non-invasive imaging test provides cross-sectional views of the retina, allowing detailed evaluation of any damage or abnormalities. - Fluorescein Angiography (for Wet AMD)
This test uses a special dye to highlight blood vessels in the retina, helping to identify leakage or neovascularization associated with wet age-related macular degeneration (AMD). - Early Detection is Crucial for Treatment Success
Detecting macular degeneration early is vital for implementing effective treatment strategies and preserving as much vision as possible.
Treatment Options
Treating Eye Floaters
Conservative Management (Most Common):
- Observation and Adaptation: Many floaters naturally settle below the line of sight over time.
- Neuroadaptation: The brain often learns to ignore its presence.
- No Treatment Typically Needed: For most individuals, floaters don’t require medical intervention.
When Treatment May Be Considered:
- Persistent, Vision-Obstructing Floaters: Significant obstruction of vision that doesn’t improve over time.
- Significant Impact on Daily Activities: Interference with tasks like reading or driving.
- Vitrectomy Surgery (Rare, Has Risks): A procedure to remove the vitreous gel in the eye, though it carries risks such as infection or retinal detachment.
- Laser Vitreolysis (Newer Option, Not for All Floaters): Use of laser technology to break up or vaporize floaters, suitable for specific cases.
Treating Macular Degeneration
Dry AMD Treatment:
- AREDS2 Vitamin Supplements: A specific formulation proven to slow progression in intermediate to late stages of dry AMD.
- Lifestyle Modifications: A healthy diet rich in leafy greens, regular exercise, and avoiding smoking can help maintain eye health.
- UV Protection: Wearing sunglasses with UV protection reduces retinal damage from harmful rays.
- Regular Monitoring: Routine check-ups to identify any progression to wet AMD.
- Low Vision Aids and Adaptive Strategies: Tools like magnifiers and specialized lighting to assist with daily activities.
Wet AMD Treatment:
- Anti-VEGF Injections (Eylea, Lucentis, Avastin): Designed to reduce abnormal blood vessel growth and leakage. Typically administered every 4-8 weeks initially.
- Photodynamic Therapy (Less Common): Combines medication with a light source to target abnormal blood vessels.
- Laser Treatment (Specific Cases): Used to seal leaking blood vessels, though this is only an option in certain situations.
- Requires Ongoing Treatment: Wet AMD management often involves consistent long-term care.
Living with AMD
- Low Vision Rehabilitation: Specialized training to maximize remaining vision and maintain independence.
- Assistive Devices: Tools like magnifying glasses or specialized lighting to improve visual functionality.
- Technology Aids: Text-to-speech programs, large font displays, and other digital devices that assist in daily life.
- Occupational Therapy for Adaptation: Guidance to adjust daily routines and activities to accommodate vision changes.
Living with Vision Changes
Practical Tips for Managing Floaters
- Avoid Fixating on Them: Try not to focus on floaters, as this can make them more distracting.
- Move Eyes to Shift Floaters: Gentle eye movements can help move floaters out of your central vision, making them less noticeable.
- Be Patient with the Adaptation Period: It may take time to adjust to having floaters; this is a normal part of the process.
- Sunglasses Can Reduce Noticeability: Wearing sunglasses, especially in bright conditions, can diminish the visibility of floaters.
- Continue Normal Activities: Floaters are typically harmless and should not interfere with your daily routine once you adjust to them.
Adapting to Macular Degeneration
- Home Modifications:
- Increased lighting, particularly task lighting, can make activities safer and easier.
- Use high-contrast color schemes to distinguish objects more clearly.
- Reduce glare and reflections by using matte finishes or glare-reducing accessories.
- Keep spaces organized to avoid potential hazards.
- Assistive Technology:
- Use digital magnifiers and closed-circuit television (CCTV) systems for reading and other detailed tasks.
- Opt for large-print books, labels, and materials to improve visual accessibility.
- Consider voice-activated devices to simplify activities like calling or setting reminders.
- Explore special computer software designed for low vision use, such as screen readers or magnification programs.
- Wearing bioptics for driving: A recent patient Mary R. said “bioptics have been the single most important device for keeping my independence. They’ve allowed me to keep driving and to see facial details again.”
- Lifestyle Adjustments:
- Learn to use peripheral vision through techniques such as eccentric viewing to complete tasks.
- Plan activities during times of optimal lighting conditions to enhance visibility.
- Don’t hesitate to ask for help from family, friends, or professionals when tasks become difficult.
- Connect with support groups or counseling services to share experiences and gain emotional support from others living with similar challenges.
Reducing AMD Risk: Evidence-Based Strategies
Implementing evidence-based strategies can effectively reduce the risk of developing age-related macular degeneration (AMD) or slow its progression. Below are key recommendations backed by research:
Diet
- Leafy green vegetables: Foods like spinach and kale are rich in lutein and zeaxanthin, which are essential nutrients for eye health.
- Omega-3 fatty acids: Regular consumption of fatty fish like salmon, mackerel, or sardines helps support retinal health.
- Colorful fruits and vegetables: Include an array of vibrant produce, such as carrots, oranges, and berries, to benefit from their antioxidants.
- Limit processed foods: Minimize intake of highly processed or fried foods that can contribute to inflammation and poor overall health.
Lifestyle
- Avoid smoking: Smoking remains the most significant modifiable risk factor for AMD. Quitting smoking significantly lowers your risk.
- Maintain a healthy weight and adopt habits that promote a balanced lifestyle.
- Exercise regularly: Aim for at least 30 minutes of moderate physical activity on most days of the week.
- Control blood pressure and cholesterol to reduce vascular stress, which can impact eye health.
Eye Protection
- Wear UV-blocking sunglasses to protect your eyes from harmful ultraviolet rays.
- Use wide-brimmed hats to offer additional sun protection when outdoors.
- Wear protective eyewear when engaging in work or sports that may pose a risk to your eyes.
Monitoring
- Schedule regular eye exams, especially if you are over 50 years old. Annual exams can help detect early signs of AMD.
- Utilize a home Amsler grid to monitor potential vision changes. This tool can help you detect symptoms of AMD progression early.
- Be aware of your family history, as genetics may play a role in AMD risk.
- Report any vision changes immediately to your eye care professional to ensure timely intervention.
By following these evidence-based practices, you can take proactive steps to safeguard your vision and overall eye health.
Frequently Asked Questions
Can eye floaters turn into macular degeneration?
No, eye floaters and macular degeneration are separate conditions that impact your vision in different ways. Floaters typically result from changes in the vitreous gel of your eye, while macular degeneration affects the retina. However, having one condition does not directly lead to the other.
How can I tell if my vision problems are from floaters or macular degeneration?
Floaters are usually seen as dark, shadowy shapes that move when your eye moves, often appearing against bright backgrounds. Macular degeneration, on the other hand, typically results in central vision loss or distortion, such as straight lines appearing wavy. An eye care professional can perform tests to distinguish between these conditions.
If I have both conditions, will treatments for one affect the other?
Generally, treatments for floaters and macular degeneration address different parts of the eye and work independently of one another. It’s essential to consult with your eye doctor to create a treatment plan tailored to both conditions.
Are floaters ever a sign of something serious?
While most floaters are harmless, the sudden onset of numerous floaters, flashes of light, or a shadow over your vision could indicate a serious issue like retinal detachment. If you experience any of these symptoms, seek medical attention immediately.
At what age should I worry about macular degeneration?
Macular degeneration is most common in people over the age of 50, and the risk increases with age. However, adopting healthy lifestyle habits and having regular eye exams can be beneficial at any age to protect your vision.
Can diet and supplements help with both conditions?
A healthy diet rich in leafy greens, omega-3 fatty acids, and antioxidants can support overall eye health. Specific supplements, like those containing lutein, zeaxanthin, and vitamins C and E, have been shown to slow the progression of age-related macular degeneration. While diet may not directly affect floaters, maintaining overall eye health can be valuable.
Will my insurance cover treatment for these conditions?
Insurance coverage can vary depending on your plan, but many policies cover medically necessary treatments for macular degeneration and serious issues related to floaters. It’s recommended to contact your insurance provider to understand the specifics of your coverage.
Conclusion
Protecting your vision is an essential part of maintaining your overall quality of life. By staying informed about age-related macular degeneration (AMD) and implementing preventative strategies, you can play an active role in preserving your eye health. Regular check-ups, healthy lifestyle choices, and early detection tools are valuable steps toward minimizing the impact of AMD. Remember, you are not alone, your eye care professional is there to guide and support you every step of the way. Taking these precautions today can make a meaningful difference for your vision tomorrow.