OCT test for macular degeneration
With the use of optical coherence tomography (OCT) technology, cross-sectional retinal pictures with semihistologic resolution may be obtained.
It enables the definition of the location and kind of changes in the retina and surrounding tissues and provides an unbiased assessment of the thickness of the retina and those structures.
With the use of these capabilities, freshly arising fluid, intraretinal or subretinal tissue, and tissue underneath the retinal pigment epithelium may all be detected (RPE).
OCT enables a more accurate and thorough investigation of anatomical structures and neovascular membrane lesions subtypes. It also gives vital information on serous (RD) retinal detachments, hemorrhages, and subretinal neovascular membranes, which are components of exudative macular degeneration.
These abilities make it easier to comprehend the variations between classic membranes, occult membranes, retinal angiomatous proliferation (RAP), and disciform scars in the disease’s natural progression and gauge how anti-vascular endothelial growth factor (VEGF) medications affect the condition.
Based on the various reflectivities of the tissue structures, the pictures are shown on a color (or gray) scale.
To put it more simply, tissues that reflect or scatter more light are depicted in red and white, respectively, whereas tissues that do the opposite are depicted in blue and black.
Light-reflecting tissues are shown as green or yellow. It should be emphasized that the hue seen in the photos does not represent the tissues themselves but rather their optical characteristics.
As a result, although the picture is fake, it accurately depicts the measured structures’ actual dimensions.
OCT’s importance in diagnosing AMD
A sophisticated and acutely sensitive examination called optical coherence tomography (OCT) utilizes light beams to produce finely detailed pictures of your eye.
OCT is like ultrasound, but with light. Light rays are focused on the tissues of your eye. The sensors of the machine then receive the light after it has been “back-reflected” or “backscattered.” The machine is able to determine the size and shape of the retinal structures it touches by the light’s bouncing “echo.”
OCT imaging may provide a three-dimensional, real-time image of your eye. This makes it easier for your ophthalmologist to detect macula damage than with other types of testing.
In addition to macular degeneration, this 2017 study found that OCT can identify glaucoma, hemorrhages, retinal detachments, and other diseases.
OCT testing is being used increasingly often to diagnose AMD. According to a 2021 study, OCT imaging is reliable and helpful for identifying a variety of macula disorders, including both wet and dry AMD.
What other disorders may OCT be used to diagnose?
OCT can aid in the diagnosis of a number of eye disorders, such as:
- Glaucoma is a rise in intraocular pressure in the eye that harms the optic nerve
- macular hole, which is a tear in the macula, swelling of the macula
- macular pucker, a bulge or wrinkle in the macula
- Vitreous traction occurs when the vitreous, gel-like material in the eye, separates from the retina and pulls on the macula.
- Diabetic retinopathy occurs when diabetes destroys blood vessels in the eye. Central serous retinopathy is an accumulation of fluid behind the retina.
- OCT is helpful for evaluating disorders involving the optic nerve since it can also examine the fibers of the optic nerve.
OCT employs light waves, therefore it cannot detect problems like thick cataracts or vitreous hemorrhage that alter how light passes through the eye.
What does AMD look like on an OCT?
The thickness of the retina may be determined via an OCT scan, and any fluid-filled regions can be found.
The choroid, a tissue layer located in the rear of the eye between the sclera (the white outer layer) and the retina, is also examined by OCT. These b lood vessels in the choroid carry oxygen and nutrients to the eye.
What OCT images can demonstrate in AMD
- Drusen, which are tiny protein and lipid buildups underneath the retina
- The retina’s structure; any new or aberrant blood vessels; and any eye hemorrhage
What OCT scans reveal about wet and dry AMD
Age-related maculopathy is characterized by the presence of confluent or soft drusen and/or regions of hyper- or hypopigmentation of the RPE, which are now thought to be a precursor to age-related macular degeneration (AMD). There is a higher risk of developing AMD when soft drusen in the macular region are connected to focal regions of pigmentary alterations (hypo- and hyperpigmentation). The accumulations of proteins, lipids, mucopolysaccharides, and other substances known as neurosensory retinal detachmenttive nodular formations, which are mostly found in Bruch’s membrane, start to show up in adulthood and tend to get bigger and more numerous over time. The drusen are the earliest AMD symptom that may be clinically seen during fundus exams. Drusen occur on OCT as RPE thickening or deformation that may produce abnormalities and undulations.
Histologically speaking, drusen are divided into two groups: soft drusen, which are deposits of granular or amorphous material thought to be AMD precursors, and hard forms, which are described as tiny hyaline deposits with demarcated edges and are thought to represent age-related low-risk alterations. Drusen can proceed to either a wet or dry atrophic type of AMD. The number, size, and confluence of drusen of the lesions determine the risk.
AMD comes in two different forms. Each kind of sign may be recognized by OCT.
The choroid, RPE, and outer retinal layers are all impacted by age-related macular degeneration (AMD). Exudative and non-exudative forms of the syndrome are separated. To avoid irreversible vision loss, exudative AMD must be identified as early as possible. The eye care professional’s objective is to identify early CNVM before subretinal fibrosis progresses and causes scarring and irreparable harm to the outer retinal layers.
Our capacity to identify early choroidal neovascular membranes (CNVM) in exudative/wet AMD has been greatly improved using OCT. The device is also employed in the monitoring of anti-vascular endothelial growth factor (VEGF) therapy efficacy. TD-OCT and SD-OCT were used in the Comparison of AMD Treatment Trials (CATT) trial to monitor the effectiveness of the treatments Avastin and Lucentis.
Dry/non-exudative AMD OCT
Depending on the drusen’s makeup, a lesion’s drusen might look hyper-reflective with certain areas of hypo-reflectivity. The drusen lies between the RPE and Bruch’s membrane, allowing Bruch’s membrane to be seen. The RPE may seem disturbed, thinner, and uneven as a result of drusen. As the disease worsens, the IZ line and EZ line may become disturbed along with the RPE, which corresponds to a decline in visual acuity.
Dry AMD
The most typical kind of AMD is dry AMD. It happens when the macula thins out and drusen deposits accumulate, gradually impairing vision.
Atrophic AMD
RPE, the outer layers of the retina, the choriocapillaris, and thick clusters of capillaries are all undergoing progressive atrophy in the macular area. RPE, outer retinal layers, choriocapillaris, and thick drusen clusters all exhibit progressive atrophy in the macular area.
The lower capacity of the atrophic retinal tissue to attenuate light causes decreases in retinal thickness and increases in the reflectivity of the RPE detachment, which allows the laser beam to penetrate deeper areas like the choroid (Figure 3). The retinal maps that show the locations with the most atrophy, gauge its size, and track advancement can be used to estimate the reduced retinal thickness and volume. Geographic atrophy (GA), the last stage of dry AMD, is a condition.
Exudative (Wet) AMD
Wet AMD: The development of new, aberrant blood vessels behind the retina may be a sign of wet AMD. Blood or fluid leakage from the blood vessels can damage the macula and speed up the onset of visual loss compared to dry AMD.
Wet age-related macular degeneration OCT
OCT, a crucial diagnostic and therapeutic tool for patients with choroidal neovascularization (CNV) enable the recognition of active neovascular membranes and, in many circumstances, the quantification of the membranes’ extent. The technology aids in the evaluation of the subfoveal area and also aids in the diagnosis of membranes known as occult choroidal neovascular (CNV) vessels, in which fluorescein angiography (FA) frequently displays perplexing patterns. OCT has also been shown to be a valuable technique for assessing the necessity for retreatment in PRN (as needed) treatment regimens and for assessing the therapy response to anti-VEGF drugs.
The disease may be dome-shaped or appear as a thin formation (fusiform or nodular), and well-defined typical CNV is seen on OCT as hyperreflective patches in contact with or in front of the RPE. In front of the active membrane, there is usually some degree of retinal edema; if the retina is thinner than normal, latent new arteries may be present. A few weeks after the initiation of CNV, only disruption, breakdown, and substantial RPE thickening are seen.
AMD impairs central vision, and those who have it may have trouble focusing on the little things that are right in front of them. Peripheral vision may continue to be the same in people.
How is the OCT performed?
An OCT is a noninvasive technique carried out in the office of your ophthalmologist or optometrist.
Before an OCT examination, ocular drops are often used to enlarge or dilate your pupils. This makes it simpler to take precise retinal pictures. For a few hours after using these drops, your eyes may be sensitive to light. Sunglasses are thus a must-have, and you should think about bringing a friend or relative who can take you home after the exam.
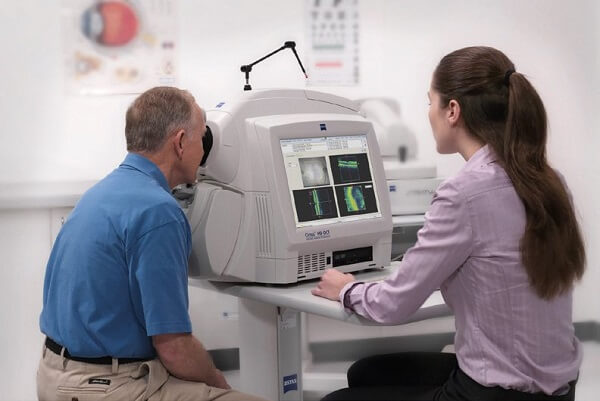
You will sit in front of a machine for the OCT test with your chin resting on a support. OCT devices resemble large desktop PCs with a few added features. On the opposite side of the device, a technician or your eye doctor will be controlling it on the monitor.
Throughout the test, keep your head steady and pay attention to your doctor’s instructions. Your eye will be scanned by the machine using laser beams. Nothing will get physically close to your eye. There shouldn’t be any discomfort, however, the exam could be a little bright and unpleasant for you.
The scan typically lasts a few seconds for each scan and there may be up to about 5 scans done.
Living with Macular Degeneration
Staying on top of the disease progression is key to keeping vision loss to a minimum. Having regular OCT tests helps to monitor the progression and determine if the treatments and preventative measures are working.
The future developments of AMD diagnosis and treatment using Macular Degeneration OCT
Recent studies have identified Bio-markers using the OCT to help predict the future progression of a patient’s disease. Different types of drusen and drusen clusters seem to help paint a picture of the direction of a patient’s disease. This combined with genetic testing is showing that there is a predictive course for which the disease may head.
Conclusion
OCT is a vital tool in monitoring and treating AMD. It is a quick and painless test that provides invaluable data to your eye doctor. If you have AMD you should be being followed by a doctor that has this equipment.
FAQ’s for Macular Degeneration OCT
Can an OCT scan detect macular degeneration?
Yes, this is now the standard of care for detecting and monitoring AMD.
What is normal macular thickness on OCT?
262.8±13.34 µm
Is an OCT eye test necessary?
No, often AMD can be diagnosed just by your doctor looking at your macula, however, it is very useful in monitoring the progression and is becoming even more valuable in predicting the future course of your disease.
How often should you have an OCT scan?
This will vary depending on your current state of the disease.
What are normal OCT results?
Normal would be average macular thickness with no drusen or fluid.
Are OCT eye scans safe?
Yes, very, it merely uses reflective light similar to an ultrasound with sound waves.