If you have vision loss and have started seeing things that are not there, like patterns, faces, or even animals, it can be terrifying. You might worry that you are losing your mind or developing dementia.
But here is the good news: You are likely experiencing a common and harmless condition called charles.bonnet syndrome (CBS), sometimes referred to as charles bonnet disease.
It is not a mental illness.
It is not a sign of cognitive decline.
It is simply your brain reacting to vision loss.
In fact, Charles Bonnet Syndrome is more common than most people realize. Studies show that up to 24.6% of vision rehabilitation patients-nearly 1 in 4 people attending low-vision clinics experience CBS. Many never hear about it until the hallucinations begin.
When your eyes stop sending clear pictures to your brain, your brain tries to help by “filling in the gaps.” Sometimes, it gets a little too creative and invents images that are not real.
This guide will explain exactly what is happening, why it is happening, and practical ways to manage it so you can reclaim your peace of mind.
What is Charles Bonnet Syndrome?
Charles Bonnet Syndrome (CBS), also known as charles bonnet disease, is a condition that causes visual hallucinations in people with healthy minds who have experienced significant vision loss. It is named after the Swiss philosopher Charles Bonnet, who first described it in 1760 after his grandfather, who was nearly blind, began describing very clear patterns and figures that weren’t there.
To clearly answer what is charles bonnet syndrome, the definition is simple:
- You have some form of vision loss (like macular degeneration).
- You see things that are not real (hallucinations).
- You know they are not real (you have “insight”).
- You do not have control over these images.
It is estimated that Charles Bonnet Syndrome affects anywhere from 10% to 40% of people with significant vision loss. However, Many people with charles bonnet syndrome never tell their doctors because they are afraid of being misdiagnosed with a psychiatric problem.
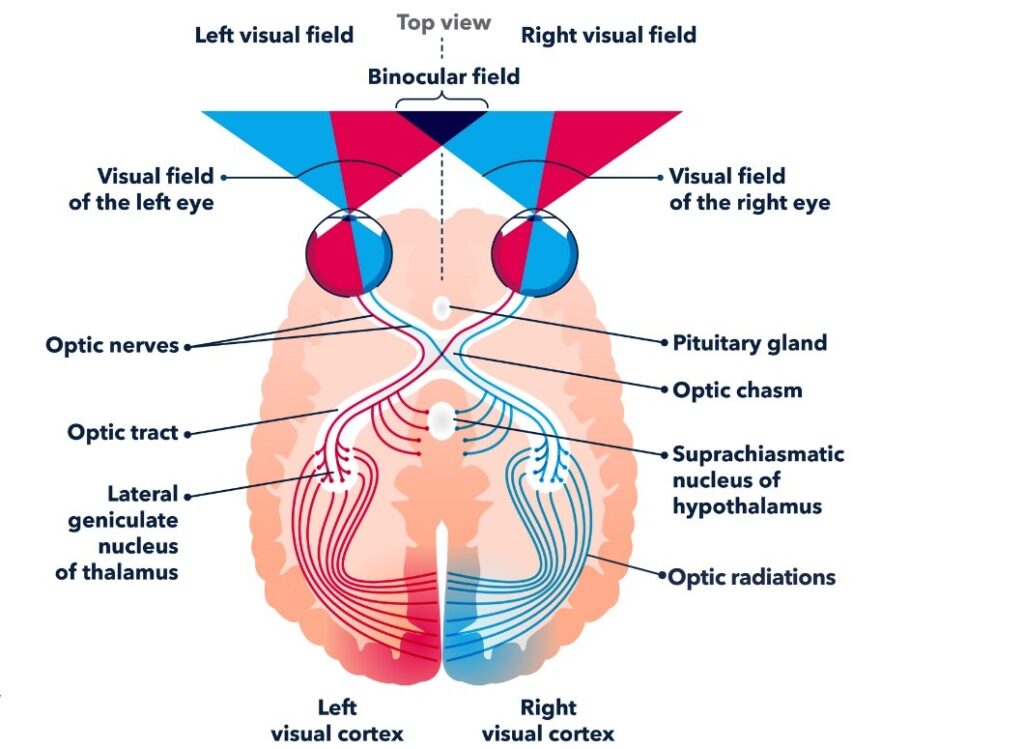
Why does the brain create these images?
Think of your brain like a television. When you have healthy eyes, they send a constant “signal” or program to your brain’s visual cortex. But when you have vision loss, that signal gets weak or stops entirely.
Instead of just showing a blank screen (static), your brain tries to tune into a channel. It turns up the volume on its internal cells, firing randomly to create images to fill the silence. This is why Charles Bonnet Syndrome is often compared to “phantom limb” pain, where an amputee feels a leg that is no longer there. Your brain is trying to see with eyes that aren’t working as well as they used to. I’ve had a few patients over the years admit that they see images that they know aren’t there, they’re relieved to know that this is very common among vision loss sufferers.
Who is at risk for Charles Bonnet Syndrome?
Charles Bonnet Syndrome can happen to anyone with vision loss, but it is most common in older adults. You don’t need to be completely blind to experience it; even moderate vision loss can trigger the condition.
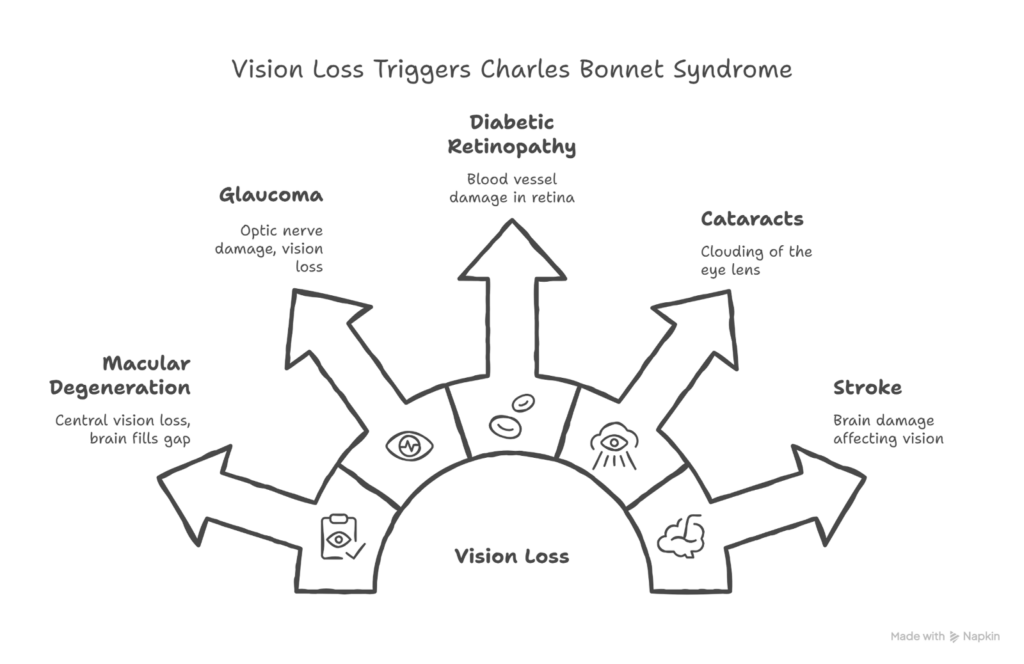
It is frequently associated with conditions that damage the eye or the optic nerve, including:
- Macular degeneration hallucinations are very common because central vision is lost, leaving a large “blind spot” for the brain to fill.
- Glaucoma
- Diabetic retinopathy
- Cataracts
- Stroke affecting vision
Factors that might make you more likely to experience Charles Bonnet hallucinations include:
- Having vision loss in both eyes (though it can happen with just one).
- A sudden drop in vision.
- Social isolation or spending a lot of time in low-stimulation environments.
- Fatigue or stress.
What do hallucinations look like?
The hallucinations caused by Charles Bonnet Syndrome can be incredibly varied. They typically fall into two main categories: simple and complex.
- Simple hallucinations
These are unclear and non-specific. They might look like:
- Geometric patterns like grids, bricks, or honeycombs.
- Repeated shapes or vivid colors.
- Flashes of light or zigzags.
- Netting or latticework covers everything you see.
- Complex charles bonnet hallucinations
These are much more detailed and can be quite startling. They might include:
- People: Strangers, historical figures, or people in costumes (like soldiers or clowns).
- Faces: Distorted, cartoon-like, or gargoyle-like faces.
- Animals: Common animals like cats and dogs, or fantastical creatures.
- Landscapes: Entire scenes of buildings, gardens, or imaginary places.
A key feature of Charles Bonnet Syndrome is that the images are strictly visual. They do not speak, make noise, or have a smell. If you see a dog barking, you won’t hear the bark.
- General Characteristics
Charles bonnet syndrome hallucinations usually:
- Charles bonnet hallucinations are always visual only (no sound, smell, or touch)*
- Appear suddenly and disappear suddenly
- May move or stay still
- Can be in color or black-and-white
- They are often very detailed and vivid
- Happen more often when you are tired, in dim lighting, or looking at blank backgrounds
Most people with CBS know the images are not real. This awareness is called “insight.”
*Important: If you also hear voices, smell things, feel things, or feel confused, you should see a doctor. That may be a different condition.
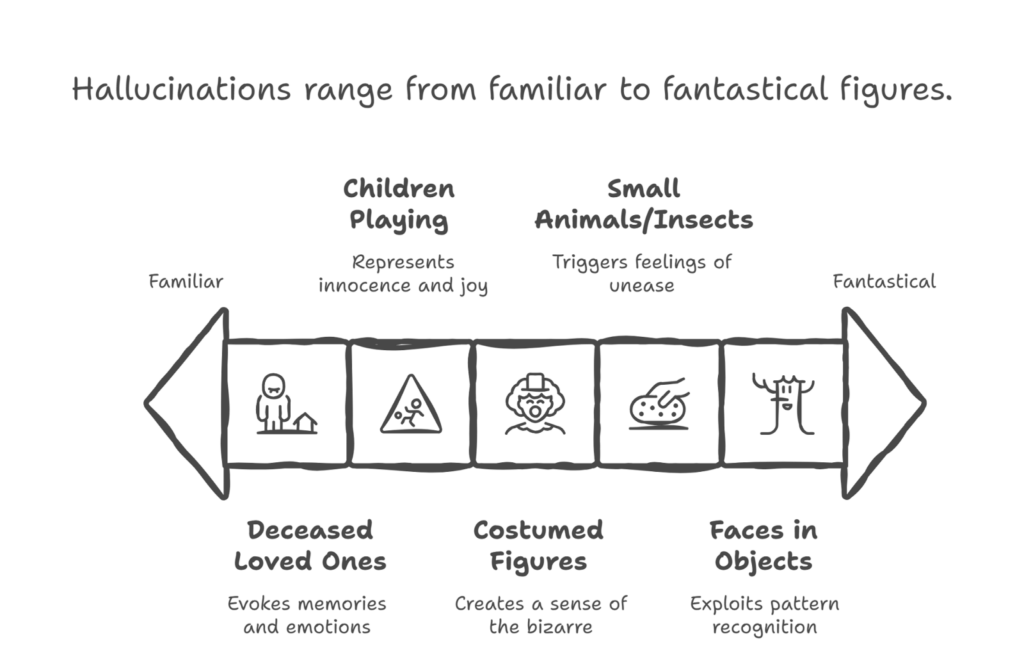
- Common Patterns
People describe seeing:
- Deceased loved ones
- Children playing
- Costumed figures (clowns, soldiers, dancers)
- Small animals or insects
- Faces in objects, similar to seeing shapes in clouds (pareidolia-like).
CBS vs Other Conditions
Understanding how Charles Bonnet syndrome (CBS) is different from other causes of hallucinations can prevent a lot of fear and confusion.
- Key Characteristics of CBS
CBS is more likely when:
- Vision loss is present (from AMD, glaucoma, diabetic retinopathy, stroke, etc.).
- Hallucinations are visual only (no voices, smells, or touch).
- Insight is intact – the person knows the images are not real.
- There is no new cognitive decline (no new memory loss or major confusion).
- There are no other new neurological symptoms (no weakness, speech trouble, or severe headache).
- Symptoms begin or worsen after vision loss starts.
- NOT Charles Bonnet Syndrome If…
You should think of other causes (and see a doctor) if:
- Auditory hallucinations (hearing voices or sounds) are present → may need psychiatric evaluation.
- There are delusions or fixed false beliefs (fully believing the images are real) → check for dementia or psychosis.
- There is memory loss or confusion → needs a thinking assessment.
- Symptoms began after recent medication changes → may be a medication side effect.
- There are hallucinations without any vision loss → more likely a neurological or psychiatric cause.
- There are flashes of light with new floaters → could signal a retinal tear or detachment (eye emergency).
- When to Seek Urgent Care?
Get urgent medical attention (same day /emergency) if you notice:
- Sudden new flashes of light with floaters.
- A curtain or shadow coming over part of your vision.
- Hearing voices or sounds along with visions.
- New confusion, disorientation, or memory problems.
- You start believing the hallucinations are real (losing insight).
- Your distress is so strong that it interferes with daily life, sleep, or safety.
- Conditions Doctors May Consider (Differential Diagnoses)
If your symptoms do not fit CBS, doctors may look for:
- Lewy body dementia (often visual hallucinations plus changes in thinking or movement).
- Alzheimer’s disease with visual symptoms.
- Medication-induced hallucinations (from certain pain meds, Parkinson’s drugs, sleep aids, etc.).
- Peduncular hallucinosis (hallucinations after certain types of stroke).
- Seizure-related hallucinations (from abnormal brain electrical activity).
charles.bonnet syndrome is a manageable and non-psychiatric condition that typically improves over time.
CBS and Macular Degeneration
- Why macular degeneration and hallucinations often occur together?
Charles Bonnet syndrome (CBS) is especially common in people with age-related macular degeneration (AMD). In hallucinations and macular degeneration, AMD damages central vision, creating a “blank” or blurred area in what individuals can see. The brain attempts to compensate for this missing information by filling in the gaps, sometimes resulting in detailed visual hallucinations. Studies suggest that CBS affects about 12–15% of individuals with AMD, and it becomes more common in advanced stages of AMD when vision loss is severe. Both dry and wet forms of AMD can lead to CBS.
- AMD-Specific Patterns
Patients experiencing CBS alongside AMD often notice visual hallucinations that align with how their vision is impacted:
- Macular degeneration hallucinations typically appear in central vision, where the damage is most significant.
- In macular degeneration and hallucinations, faces may appear where none exist, as the brain’s face-recognition system tries to fill in gaps.
- During macular degeneration hallucinations, reading may be challenging, with extra letters or words seemingly appearing on the page.
- Blank backgrounds often cause macular degeneration hallucinations, such as walls, which can suddenly display intricate images, patterns, or even people.
- Stages of AMD and CBS
The likelihood of experiencing CBS changes depending on the stage of AMD:
- Early AMD: CBS is rare at this stage.
- Intermediate AMD: CBS may appear gradually as vision starts to decline.
- Advanced AMD or severe vision loss: CBS is most common in this stage. A sudden sharp decrease in vision, such as a bleed from wet AMD, can cause the sudden onset of CBS symptoms.
- Diabetes Connection
CBS is not exclusive to AMD; people with diabetic retinopathy may also experience it. Conditions like diabetic macular edema (swelling in the macula) can lead to visual hallucinations. Maintaining good blood sugar control might help stabilize vision changes and potentially reduce the frequency of CBS episodes. In my experience, unless a diabetic patient has a a severe central vision loss, they don’t tend to have as many episodes as AMD patients.
- Post-Treatment CBS
Changes in vision after treatment can influence CBS:
- Hallucinations may temporarily worsen following injections or procedures, especially if vision fluctuates.
- If vision improves with treatment, CBS symptoms may become less intense or frequent.
- For some individuals, CBS may persist despite treatment improvements but often becomes more manageable over time.
Coping Strategies & Treatments
No “Cure,” But Charles Bonnet Syndrome Treatment and management are possible
There is no specific pill or surgery that “cures” Charles Bonnet Syndrome (CBS), but many people learn to reduce episodes and feel less frightened by using simple strategies. Over time, the brain often adapts, and hallucinations become weaker or less frequent.
- Immediate charles bonnet treatment techniques
Eye Movement Exercise – a simple charles bonnet treatment approach
This simple eye exercise can stop or shorten an episode for some people:
- Pick two points on a wall about 3 feet apart.
- Keep your head still and eyes open.
- Move your eyes quickly left and right between the two points for 15–30 seconds.
- Pause and see if the hallucination fades.
- If it is still there, you can repeat it once or twice.
This technique appears to help roughly 30% of people with CBS and can be repeated for each episode.
- Other Immediate Responses
When a hallucination appears, try:
- Looking directly at it (this often makes it fade).
- Changing the lighting – brighter is usually better.
- Blinking rapidly several times.
- Looking away or briefly closing your eyes, then reopening.
- Moving to a different room or environment.
- Starting a conversation or simple activity to shift attention.
- Lifestyle Modifications
Lifestyle Modifications as part of charles bonnet treatment. Small daily changes can lower how often hallucinations occur:
- Reduce stress, as stress can make episodes worse.
- Get adequate sleep; fatigue is a common cause.
- Avoid social isolation – talk to family, friends, or support groups.
- Keep your home well-lit, especially in the evening.
- Minimize blank walls or empty surfaces by adding pictures, patterns, or textures.
- Stay mentally and physically active with hobbies, gentle exercise, and social activities.
- Improving Vision = Reducing CBS
The more useful visual information the brain receives, the less it needs to “fill in” with hallucinations. Low vision aids can help:
- Electronic magnifiers for reading and near tasks.
- Better lighting to reduce dark or “blank” areas in your vision.
- TV or screen magnifiers to provide more detailed stimulation.
- Audiobooks and audio materials to keep the brain engaged in a different way.
Always try to optimize remaining vision with glasses, low vision devices, and treatment for the underlying condition (such as AMD injections or diabetic eye care).
- Charles Bonnet Syndrome Treatment Options (If Symptoms Are Severe)
Medication is usually a last resort, reserved for very distressing cases:
- Antipsychotics (e.g., risperidone, olanzapine):
- Used rarely and only when hallucinations are extremely upsetting.
- Given at low doses with careful monitoring because of side effects.
- SSRIs (antidepressants):
- May help if there is significant anxiety or depression.
- No strong proof they directly stop CBS, but they can improve overall coping.
- Anticonvulsants (such as gabapentin or carbamazepine):
- Occasionally tried.
- Evidence is limited, and results vary between individuals.
Always discuss risks and benefits with a doctor before starting any medication.
- Vision Rehabilitation
Vision rehab can be just as important as medicine:
- Training to use remaining vision more efficiently.
- Reducing time spent staring into “blank” areas that can causeCBS.
- Occupational therapy techniques to make daily tasks easier and safer.
- Eccentric viewing training (learning to use healthy parts of the retina, especially helpful in AMD).
- Support Groups
You are not alone in this experience. Support can make a big difference:
- Talking about CBS often reduces fear and shame.
- Hearing others’ stories normalizes the condition.
- You can share and learn coping strategies that work in real life.
- Options include online communities and in-person groups through eye clinics or low vision centers.
Living With CBS
- Emotional Impact
When Charles Bonnet Syndrome (CBS) first appears, it is often frightening and confusing. Many people secretly worry they are “going crazy.” This fear, plus embarrassment about talking about the hallucinations, can lead to pulling back from friends and activities. If no one explains what is happening, this stress and isolation can increase the risk of depression.
- Education about charles bonnet syndrome reduces distress
Understanding what is charles bonnet syndrome and that it is caused by vision loss, not mental illness, usually brings huge relief. Knowing that it is common in people with vision loss reduces shame. Sharing this information with family or caregivers helps everyone react more calmly and normalizes the experience.
- Talking to Family/Caregivers
Explain CBS in simple terms: “My vision loss causes my brain to create images. I know they are not real.” Ask loved ones not to play along, but to gently acknowledge that you are seeing something they are not. Decide together what to do when you feel distressed versus when you are coping well and just want them to ignore it.
- Daily Life Management
You can plan around CBS. Try to anticipate triggers like blank walls, fatigue, and dim light. Keep your surroundings bright and interesting, maintain social connections, and use humor when it feels right.
- Quality of Life and Prognosis
Most people adapt within months. Hallucinations often decrease over time as the brain adjusts to vision loss. Low vision aids can restore independence and confidence. On average, CBS lasts about 18 months, though it can persist longer. For many people, frequency and intensity gradually drop, and some report that episodes stop completely.
For long-term follow-up, about 80% of people report improvement over five years.
When CBS Requires Medical Attention?
- Routine Discussion (Next Eye Appointment)
Even if your hallucinations are mild, it’s important to mention CBS at your next eye appointment. Tell your eye doctor:
- How often the hallucinations happen and how long they last
- What types you see (patterns, people, animals, scenes)
Ask about a low vision evaluation to see if devices or lighting changes could help. If you have macular degeneration, your doctor can also work on optimizing AMD treatment, which may reduce CBS by improving your vision or stabilizing it.
- Urgent Evaluation Needed
You should seek urgent medical help (same day or soon) if any of the following occur:
- The distress from hallucinations is interfering with daily life
- You notice growing depression or anxiety
- You start believing the hallucinations are real (loss of insight)
- You have thoughts of self-harm or worry you might be unsafe
- You cannot function normally at home or outside
- Family or caregivers are concerned about your safety
- Emergency (Call 911 / Local Emergency Number)
Call 911 or your local emergency number immediately if:
- You have suicidal thoughts or plans
- You are threatening to harm others
- There is a complete break with reality (severe confusion, no insight)
- A serious medical emergency happens at the same time (e.g., stroke symptoms, chest pain)
- Who to See?
Different professionals can help with different parts of CBS:
- Ophthalmologist – checks for retinal or other eye problems and works to optimize your vision
- Low vision specialist – helps you maximize remaining vision and reduce visual “blank spots” that can trigger CBS
- Psychiatrist or psychologist – supports you if there is severe distress, anxiety, depression, or if medicines are being considered
- Primary care doctor – reviews your overall health and medications to see if anything else may be contributing to hallucinations or mood changes
Prompt attention and medical support can make a significant difference in managing CBS effectively.
Low Vision Aids & CBS Prevention
- How Better Vision Reduces Hallucinations?
Charles Bonnet syndrome happens when the brain does not get enough clear visual information and starts to “fill in the gaps.” When you improve the quality of what you can see, the brain has less empty space to decorate with hallucinations. More visual input = less brain “filling in.”
- Magnification helps the visual cortex work with real images instead of noise. Devices like magnifying glasses or electronic readers can provide clearer details, reducing strain and improving focus on objects, reading materials, or everyday tasks.
- Engaging in reading and visual activities keeps the brain busy and focused, reducing idle time that could otherwise allow CBS-related hallucinations to arise.
- Social connection is also important. Talking, spending time with loved ones, or joining support groups reduces isolation, which can make CBS episodes feel less intense and less scary.
Better vision aids do not just improve how much you see, they improve brain function and emotional well-being, playing a key role in managing conditions like CBS.
- Recommended Low Vision Aids for CBS Reduction for AMD Patients
- Electronic Magnifiers (CCTVs)
- Provide clear, magnified images for reading and near work.
- Reduce time spent staring into a blank central area.
- Help the brain engage properly with text and pictures.
Explore electronic magnifiers here.
- Lighting
- Bright task lighting is crucial for reading, cooking, hobbies, and moving around safely.
- Reduces dim conditions that can trigger or worsen CBS episodes.
- Full-spectrum bulbs often give more comfort, even light.
Browse lighting solutions here.
- Portable Magnifiers
- Help you stay engaged with labels, menus, signs, and small print.
- Reduce “blank staring” into space, which can invite hallucinations.
- Support independence at home and in public places.
Check handheld magnifiers here.
- Audio Devices
- Audiobooks and podcasts reduce the demand on your eyes, while still stimulating your brain.
- They supplement visual aids, rather than replacing them.
- Screen readers can help you use computers and smartphones with less visual strain.
- Creating Visual Stimulation
You can shape your surroundings to be friendlier for CBS:
- Reduce blank walls by adding art, photos, patterns, or textured décor.
- Keep a TV or radio on in the background if silence makes you focus more on the images.
- Change where you sit and what you look at during the day. Don’t stay in the same spot for hours.
- Choose activities that use your vision: puzzles, crafts, cooking, sorting objects, or watching shows.
- Low Vision Rehabilitation
Low vision rehab brings everything together:
- A professional assessment to understand your remaining vision.
- Training on how to use devices (magnifiers, lighting, electronic aids) correctly and comfortably.
- Techniques to maximize remaining vision so you rely less on “blank” areas. This reduces the opportunities for CBS to be triggered.
Book a consultation here.
Success Stories
Many people find that once they start using the right low vision aids and strategies:
- Their CBS episodes become less frequent or less intense.
- Quality of life improves when they can read, cook, or enjoy hobbies again.
- Regaining independence reduces isolation and fear.
- Staying mentally and physically active often helps hallucinations fade into the background, becoming a smaller and more manageable part of life.
Pam B. a low vision patient reported that once she started using her bioptic telescopes to see things more clearly that her occurrences were greatly reduced due to the magnification filling in the blanks better.
Frequently Asked Questions (FAQs)
Q1: Is Charles Bonnet syndrome a sign of dementia or mental illness?
A: No. CBS is not dementia and not a mental illness. It is a vision-related condition where the brain reacts to reduced visual input by creating images. Most people with CBS have clear thinking and know the images are not real.
Q2: Will my hallucinations ever go away?
A: In many people, hallucinations fade over time. They often decrease over 12–18 months as the brain adapts to vision loss. For some, they may last longer, but the frequency and intensity usually lessen.
Q3: Should I tell my doctor about the hallucinations?
A: Yes. You should always tell your eye doctor or primary doctor about hallucinations. This helps them document your symptoms, check for other possible causes, and guide you to low vision services and support.
Q4: Can improving my vision stop the hallucinations?
A: Improving your vision often reduces hallucinations. Low vision aids (like magnifiers and better lighting) give the brain more real visual information, so it has less need to “fill in the gaps.”
Q5: Are hallucinations dangerous?
A: CBS hallucinations are not physically dangerous and do not harm the eyes or brain. However, they can be emotionally upsetting or tiring. Learning what CBS is, and using coping strategies, usually makes them easier to live with.
Q6: Why do I see specific things like children or animals?
A: Your brain often uses stored visual memories, things you have seen many times before. That is why many people report seeing children, faces, animals, or familiar scenes. These patterns are common across many CBS patients.
Q7: Do hallucinations mean my AMD is getting worse?
A: Not always. CBS means there is significant vision loss, but it does not automatically mean your AMD is suddenly getting worse. Your eye doctor can check whether your AMD is stable or changing.
Q8: Can medication help with Charles Bonnet syndrome?
A: Most people manage CBS with education and simple techniques, not medication. In rare, very distressing cases, a doctor may consider medicines such as antipsychotics or antidepressants, but these are used carefully and only when needed.
Q9: Will I have this forever?
A: Probably not in the same way. Many people see clear improvement over time. CBS can persist in some, but episodes often become shorter, less frequent, and easier to ignore as the brain adapts and coping skills improve.
Q10: How do I explain this to my family?
A: You can say something like:
“My eyes have vision loss, so my brain sometimes creates images to fill the gaps. This is called Charles Bonnet syndrome. I know the images are not real. It’s not a mental illness or dementia.”
Sharing articles or leaflets, and bringing family to appointments, can also help them understand and support you.
Charles Bonnet syndrome is a condition that can often be improved with time, understanding, and the right coping techniques.
Resources & Support
Living with Charles Bonnet syndrome is easier when you know where to turn for information and connection. These resources can help you and your family feel less alone.
- Organizations
These groups offer information, helplines, and services related to vision loss and CBS:
- Charles Bonnet Syndrome Foundation
- Macular Society (UK) – excellent information on CBS and AMD
- American Foundation for the Blind
- Prevent Blindness America
- Local vision rehabilitation centers (often linked to hospitals, eye clinics, or national blindness organizations)
- Online Support
Many people find comfort in hearing from others who experience CBS or vision loss:
- CBS-specific support groups (often hosted by charities or hospitals)
- AMD patient communities
- Vision loss forums
- Facebook groups for CBS and macular degeneration
These spaces allow you to share tips, ask questions, and feel understood.
- Professional Help
- Find a low vision specialist: [link]
- Ask about counseling to help with adjustment, anxiety, or depression
- Join support groups (local or online) through clinics, charities, or rehab centers
- Educational Materials
- Patient handouts you can give to family and caregivers
- Videos explaining CBS in simple language
- Real-life testimonials from others living with CBS, which can be reassuring and practical
Your eye clinic, low vision service, or national vision charity is often the best starting point to access these resources.
Conclusion
Charles Bonnet Syndrome is common, not dangerous, and usually manageable. It happens when the brain tries to fill in the gaps from vision loss, it doesn’t mean you’re “losing your mind.” If you see patterns, faces, or scenes that aren’t there, you are not alone.
The most important step is to talk to your doctor to rule out other causes. From there, practicing the coping strategies in this guide and using low vision aids can help reduce triggers. For most people experiencing hallucinations and macular degeneration, CBS becomes easier to live with as the brain adapts.
At Low Vision Aids, our goal is to help you maximize your remaining vision and reduce CBS triggers. Take the next step by scheduling a low vision evaluation to live more confidently with CBS.