Is diabetic retinopathy reversible?
Chronic diabetes that damages the blood vessels in the retina is known as diabetic retinopathy. While vision loss cannot be totally prevented or reversed, it can sometimes be prevented or mitigated with early detection and appropriate therapy.
The main objective of treatment for diabetic retinopathy is to maintain healthy blood pressure, cholesterol, and blood sugar levels. Working closely with a healthcare team, which may include a primary care physician, an endocrinologist, and an ophthalmologist, is often required for this. Effective diabetes management can slow the development of retinopathy and protect vision.
Laser therapy or other surgical techniques may occasionally be used to treat particular complications of diabetic retinopathy, such as leaking blood vessels or abnormal growth of new blood vessels if the condition is diagnosed early and the blood sugar levels are effectively controlled.
To identify any early warning symptoms of diabetic retinopathy or other eye-related issues, it’s crucial for people with diabetes to get routine eye exams, at least once a year or as advised by their healthcare professional. Early diagnosis and treatment can save vision and stop additional harm.
Working closely with healthcare providers to control the disease and receive the proper eye care will help to lessen the effects of diabetic retinopathy if you or someone you love has diabetes.
What causes diabetic retinopathy?
Diabetes-related diabetic retinopathy is brought on by persistently elevated blood sugar levels. The precise mechanisms that cause diabetic retinopathy to develop are complicated and not yet entirely understood. But there are a few crucial elements that support its development:
Damage to blood vessels
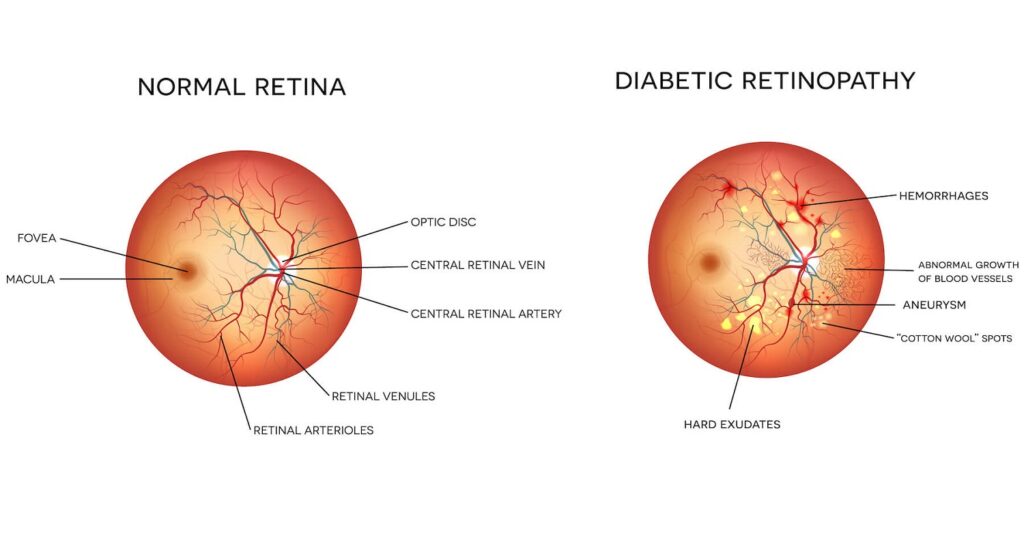
Blood vessels all over the body, including those in the retina, can be harmed by high blood sugar levels. Blood and other fluids flow into the surrounding tissues as a result of this damage, which weakens and narrows the blood vessels in the retina over time.
Formation of abnormal blood vessels
The body may attempt to make up for the damaged blood vessels by developing new blood vessels. These new blood vessels, however, are fragile and irregular, which increases leakage and could result in bleeding into the retina.
Chronically high blood sugar levels can result in inflammation and oxidative stress, both of which exacerbate the damage done to blood vessels and retinal cells. This may hasten the progression of diabetic retinopathy even more.
Impairment of blood flow
Diabetes can compromise the retina’s regular blood flow. The retina loses oxygen and vital nutrients as a result of decreased blood flow, which causes tissue damage and vision loss.
These elements work together to cause the retina to undergo a variety of changes including swelling (macular edema), the development of deposits (exudates), bleeding (hemorrhages), and the proliferation of abnormal blood vessels (proliferative diabetic retinopathy). If left untreated, these alterations might cause vision impairment and eventually result in severe vision loss or even blindness.
Remember that not all people with diabetes will get diabetic retinopathy. Adequate management of other diabetes-related disorders, such as high blood pressure and high cholesterol, can help lower the risk and slow the development of diabetic retinopathy. Strict blood sugar control, routine eye exams, and treatment of these conditions can all help.
What are the many diabetic retinopathy stages, and can the retinal damage be reversed at each stage?
According to the severity of the illness, diabetic retinopathy is often divided into many stages. These phases consist of:
Mild Nonproliferative Diabetic Retinopathy (NPDR)
In this early stage, tiny regions of the retina’s blood vessels may weaken and leak, which might result in the development of microaneurysms. There may not yet be any observable symptoms or eyesight changes.
Moderate NPDR
The retina receives less blood as the condition worsens because more blood vessels are clogged. Cotton-wool spots (patches of nerve fiber layer infarcts) and retinal ischemia (lack of oxygen) may develop as a result of this. At this point, vision may begin to be impacted.
Severe NPDR
The blood supply to the retina continues to decline at this stage as a considerable number of blood vessels get blocked. Neovascularization, the growth of abnormal blood vessels, may result in the retina’s or the optic nerve’s surface as a result of this.
Diabetic retinopathy in its advanced stage is known as proliferative diabetic retinopathy (PDR). It happens when the abnormal blood vessels that have grown and extended into the vitreous gel in the center of the eye as a result of the previous stage. Due to the fragility and bleeding risk of these new blood vessels, vision loss or even blindness may occur.
Now, in terms of reversing retinal damage at each stage:
Mild NPDR
The extent of the retinal damage may be negligible or nonexistent at this point. The growth of retinopathy can be slowed down or even stopped with proper care of diabetes, including blood sugar control, blood pressure management, and routine eye exams.
Moderate NPDR
Although the extent of the retinal damage is greater at this stage, appropriate management can still help halt the disease’s growth and stop additional damage. Specific consequences, such as macular edema, may require treatments like laser photocoagulation or injections of anti-VEGF drugs.
Severe NPDR and PDR
At this stage, preventing additional vision loss is more important than repairing the damage already done. Treatment options may include vitrectomy (surgical removal of the vitreous gel) for severe bleeding or tractional retinal detachment, laser therapy (pan-retinal photocoagulation) to stop the formation of aberrant blood vessels, and anti-VEGF injections to treat macular edema.
It’s important to remember that while diabetic retinopathy’s effects on the retina cannot be fully reversed, early detection, appropriate diabetes management, and prompt intervention can help reduce the disease’s progression, preserve eyesight, and prevent catastrophic vision loss. Effective management of diabetic retinopathy requires frequent eye exams and constant communication with medical specialists.
Can you restore vision from diabetic retinopathy?
Depending on the degree of retinal damage and the stage of the disease, diabetic retinopathy patients may be able to regain some vision. Remember that diabetic retinopathy is a chronic and progressive disease and that once vision loss starts, it might not entirely recover.
However, vision loss can be limited and the disease’s further course can be slowed down with early detection and the right care. Regular eye exams and proper blood sugar, blood pressure, and cholesterol management are essential for treating diabetic retinopathy and preserving vision.
In some instances, diabetic retinopathy-related problems including macular edema or retinal detachment may be treated with laser therapy, anti-VEGF drug injections, or vitrectomy surgery. In some cases, these treatments may result in a partial improvement in eyesight while attempting to stop additional vision loss.
It’s vital to seek the advice of an ophthalmologist or retina expert who can evaluate the patient’s unique situation and offer suitable treatments based on the degree and stage of diabetic retinopathy.
The level of retinal damage, the duration of the condition, and individual variances are just a few of the variables that can affect how well a treatment works and whether or not eyesight can become better. To increase the likelihood of maintaining and enhancing vision, it is always advisable to seek prompt medical attention and heed the advice of healthcare professionals.
Reversing diabetic retinopathy naturally
The growth of diabetic retinopathy can be slowed down naturally, there are a number of lifestyle and self-care practices that may aid in reversing diabetic retinopathy. Here are a few suggestions:
Strict blood sugar management
In order to effectively manage diabetic retinopathy, blood sugar levels must be kept under strict control. Maintain a healthy diet, engage in regular exercise, and take prescribed medications or insulin as instructed. These are just a few of your healthcare provider’s suggestions for managing diabetes.
Can diabetic retinopathy be reversed with diet?
A diet high in vegetables, whole grains (low carb is best), lean proteins, and healthy fats for a healthy diet. Consume processed foods, sweet drinks, and foods high in saturated and trans fats in moderation, and eliminate them if you can. Much of the early damage can be healed if you change your diet and control your inflammation and blood sugar.
Exercise on a regular basis
Follow your healthcare provider’s advice and partake in regular physical activity. Exercise can enhance blood sugar regulation, blood flow, and general health, all of which may slow the development of diabetic retinopathy.
Management of blood pressure and cholesterol
The development of diabetic retinopathy can be accelerated by high blood pressure and high cholesterol levels. Adapt your lifestyle, take prescribed drugs, or use a mix of the two as directed by your doctor to treat these disorders.
Regular eye exams are crucial for early detection and prompt intervention since diabetic retinopathy frequently develops without any early symptoms. A full eye exam should be scheduled at least once a year, or as your eye care specialist may advise.
Limit alcohol intake and refrain from smoking: Smoking increases the risk of various eye disorders and exacerbates the consequences of diabetic retinopathy. If you smoke, you might want to stop, and you should also limit your alcohol intake because too much alcohol might harm your eyes.
While these steps can manage diabetic retinopathy and slow down its advancement, they might not be able to repair already-done retinal damage. Working closely with your healthcare team, which should include an ophthalmologist or retina expert, is advised in order to create a personalized treatment plan and obtain the necessary medical interventions.
How can you halt the progression of diabetic retinopathy?
To successfully manage your diabetes and keep up your overall health in order to stop or slow the onset of diabetic retinopathy, here are some tips:
Keep your blood sugar under strict control
Keep your blood sugar under strict control by regularly checking it and managing it to stay within the goal range advised by your healthcare practitioner. This frequently includes maintaining a nutritious diet, getting regular exercise, taking prescribed drugs or insulin as instructed, and routinely checking blood sugar levels.
Control your blood pressure
Control your blood pressure because it can make diabetic retinopathy worse. Follow the advice of your doctor to maintain a healthy blood pressure level through lifestyle changes (such as a low-sodium diet, frequent exercise, and stress management) and medication, if required.
Control cholesterol levels
The development of diabetic retinopathy might also be facilitated by high cholesterol levels. Adopt a heart-healthy diet, engage in regular exercise, and, if your doctor prescribes it, follow their instructions when taking cholesterol-lowering medicine.
Attend routine eye checkups
Routine, thorough eye exams are essential for the early detection and management of diabetic retinopathy. These tests can aid in spotting any indications of retinal abnormalities and enable prompt action. A minimum of once a year, or as indicated by your eye care specialist, is recommended for eye exams.
Follow prescribed therapies
Your eye care expert may advise treatments like laser therapy, injections of anti-VEGF drugs, or other surgical interventions if they identify particular problems of diabetic retinopathy, such as macular edema or aberrant blood vessel growth. Implementing these treatments as prescribed can aid in managing and halting the disease’s progression.
Adopt a healthy lifestyle
Adopt a healthy lifestyle by getting regular exercise, controlling your weight, eating a balanced diet that is high in fruits, vegetables, whole grains, and lean proteins, quitting smoking, and drinking in moderation. Your whole health, including the treatment of diabetic retinopathy, can benefit from these lifestyle decisions.
Can glasses correct retinopathy?
The underlying retinal damage brought on by diabetic retinopathy cannot be effectively treated by glasses or corrective lenses, such as prescription eyeglasses or contact lenses. Damage to the retina’s blood vessels and tissues, or retinal retinopathy, impairs the brain’s ability to receive light signals.
However, refractive errors or focusing issues that may also be present in conjunction with diabetic retinopathy can be compensated for by glasses or contact lenses, which can help vision. Due to changes in the shape of the eye or the presence of other eye disorders, some people with diabetic retinopathy may develop refractive alterations, such as nearsightedness or farsightedness. By correcting for these refractive defects, the use of the proper prescription eyeglasses or contact lenses can aid in providing sharper vision.
In addition, specialized therapies or interventions can be required to address related problems such as cataracts or macular edema and enhance vision. To improve visual function in these situations, glasses or contact lenses may be recommended as part of the overall care strategy.
Summary
Keep in mind that managing diabetic retinopathy requires cooperation between you and your medical team. To ensure that your disease is properly monitored and managed, schedule regular consultations with your healthcare practitioner, including an ophthalmologist or retina specialist.