Drusen and macular degeneration, are they the same thing?
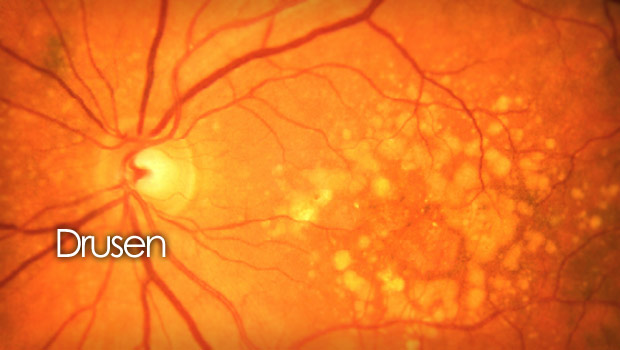
The distinguishing characteristic of macular degeneration is drusen. An ophthalmologist can identify these little yellow or white patches on the retina via retinal photography or during a dilated eye exam. A person is termed to have early age-related macular degeneration if they have more than a few tiny drusen (AMD). Frequently, people with drusen may not show any symptoms. Instead, the presence of these deposits raises the possibility of future eyesight loss to some extent. A complete eye exam is the only method to determine for sure if you have drusen.
What is Drusen?
Retinal drusen, which are comprised of proteins and a form of fat known as lipids, are the yellow spots that may be seen under the retina of your eye. The layer of cells that lines the inner surface of the back of your eye, known as the retina, is what transmits messages to your brain and gives you the ability to see.
Proteins, polysaccharides, glycosaminoglycans, lipids, amyloid, and complement factors that are produced as a result of inflammatory and immunological reactions to RPE cell injury make up drusen deposits. Continuous exposure to light causes reactive oxygen production and oxidative stress at the RPE/Bruch’s membrane junction, which clearly shows this damage.
Drusen may also be deposited from the systemic circulation and choroidal vasculature.
The Bruch’s membrane thickens and loses permeability as a result of the buildup of RPE waste products and other kinds of cellular debris. Dysfunction results from this influencing the transport of nutrients and waste materials between the RPE and choroidal circulation. This malfunction manifests clinically later on in the process of the disease as drusen.
What Is AMD or Macular Degeneration?
At the back of the eye is the retina, which is sensitive to light. The retina of the eye has a macula in the middle. It is the retinal structure that is most responsive. It makes little details visible. Outside of the Macula is the peripheral retina, which is responsible for your peripheral or side vision. Electrical impulses are converted from light or a picture by the retina. The brain then receives these electrical signals. A condition known as macular degeneration affects the eyes and causes damage to the macula as well as loss of central vision. It occurs in wet and dry forms. 90% of age-related macular degeneration is caused by dry macular degeneration, which is more prevalent (AMD).
In the US, macular degeneration, which affects more than 10 million people, is the primary cause of blindness. It gets worse as you get older, with most occurrences happening between the ages of 75 and 80.
Some people may not have issues with little drusen, but bigger drusen can raise your chance of developing age-related macular degeneration (AMD). Drusen may indicate that age-related macular degeneration is already present.
The cells of the macula, a section of the retina, begin to deteriorate due to aging in age-related macular degeneration. The initial stage is dry macular degeneration. A more severe variation of the disease is wet macular degeneration.
Types of drusen
Drusen, sometimes known as drusen bodies, are an accumulation of proteins, lipids, and cellular debris. They are tiny and have a yellow or golden Appearance.
The size and number of Drusen fluctuate. They consist of:
Hard Drusen
Small, rounded, and well-defined deposits are known as hard drusen. Future vision loss is less likely if the drusen are hard than if they are soft.
Cuticular Drusen
Cuticular drusen, which are identical to hard drusen but more abundant and commonly coalesce to produce bigger drusen deposits,
Soft Drusen
Soft drusen are larger, have soft undefined borders, and have elevations and they have a dome-like form. They have a light yellow or grayish-white hue. Future vision loss is more likely if you have a high number of large or medium-sized soft drusen.
Optic Nerve Head Drusen
Optic disc drusen (ODD) is a genetic abnormality in which the optic nerve head develops calcified protein deposits. About 70% of the time, they are typically bilateral. Although these drusen often do not affect vision, certain individuals may experience loss of peripheral vision. They are more common in younger people than AMD-related drusen and are unrelated to aging. ODD has no known cure, however vasoactive therapies like pentoxifylline and reducing intraocular pressure, which acts as a neuroprotective treatment, have shown effectiveness in managing this disorder.
Peripheral Drusen
The macula or center area of the retina contains drusen bodies, which are more worrisome than drusen bodies on the peripheral retina. The fovea, a region of the macula where the best visual acuity arises, is where the fovea is located. Hard drusen can be discovered in the central or peripheral retina because they are frequently extensive. Cuticular drusen are comparable to this. A factor in why soft drusen have a higher chance of developing into AMD is that they are more likely to be found in the central retina or macula.
Symptoms of Drusen
The majority of drusen sufferers are symptom-free. Often, they are accidentally discovered during a normal eye checkup. A few little drusen are not a sign of an eye condition. However, if a lot of bigger drusen are present as a symptom of dry age-related macular degeneration (AMD). Hazy vision, trouble seeing when switching from high to low light, and a blank or fuzzy patch in your center vision are all signs of AMD.
Additionally, optic nerve drusen frequently go unnoticed. However, some individuals with optic nerve drusen report vision issues, such as transient flickering or graying out of their vision and loss of peripheral (side) vision.
Risk Factors for Drusen?
Drusen are often related to aging and are most frequently observed in adults 60 years of age and older. Drusen and age-related macular degeneration are more common in Caucasians (white people) (AMD). A large druse is related to AMD. A family history of the condition, smoking, and race are risk factors for AMD. Obesity, high cholesterol (fat in the bloodstream), and high blood pressure are other risk factors.
White persons and those with a family history of drusen are also more likely to acquire optic nerve drusen.
How does macular degeneration start?
Wet macular degeneration happens when irregular blood vessels develop underneath the macula, behind the retina. These brand-new blood vessels frequently break and leak fluid and blood. The macula is elevated from its natural position by the blood and fluid. Loss of central vision often happens fast.
Dry macular degeneration happens when the macula’s light-sensitive cells gradually deteriorate due to the buildup of drusen or due to the atrophy of macular cells. The Macula becomes thinner. Gradually, center vision starts to fade.
Other Types of AMD
The hereditary macular dystrophies Doynes honeycomb retinal dystrophy (DHRD) and Malattia Leventinese (ML) are both characterized by the presence of drusen on the macula. In ML, the drusen are distributed in a radial pattern from the fovea centralis, whereas in DHRD, they are situated around the optic nerve head.
With an incidence of 1 in 8000–10,000, Stargardt disease (STGD) is the most common autosomal recessive macular dystrophy in children and young adults. It can appear in late adulthood on occasion. The macular has a bronze-beaten look, which causes gradual bilateral vision impairment, and this is one of the clinical signs of Stargardt’s illness.
A mutation taking place in the RPE gene BESTROPHIN causes Best disease, also known as best macular dystrophy (BMD), which is a kind of macular degeneration (BEST1). This causes a buildup of material that resembles lipofuscin in the RPE, which results in the degeneration of the RPE and photoreceptors. The best disease cannot be treated medically or surgically, however anti-VEGF medication has been demonstrated to be effective in improving symptoms. Best vitelliform macular dystrophy (BVMD), Adult vitelliform macular dystrophy (AVMD), and autosomal dominant vitreoretinochoroidopathy are the subtypes of Best disease (ADVIRC). Drusen are present on the macula in several disease states, and central vision gradually declines.
Treatment
People who are over 60 are more likely to develop retinal drusen. Some folks could have no issues at all with little drusen. Not knowing whether you’ll be the lucky one to not have any problems is a gamble, so prevention is key.
Vitamins
If age-related macular degeneration progresses to a severe level, you risk losing your eyesight. The AREDS2 formula vitamins, which can delay the progression of your ailment to an advanced stage by roughly 25%, may be prescribed by your doctor if you have a lot of large and medium-sized drusen.
Age-Related Eye Disease Study (AREDS), a clinical experiment conducted by the NIH, suggests taking the vitamins in the AREDS2 formula. The study’s findings indicate that taking these vitamins can lower your chance of developing the condition by up to 19% and/or your risk of losing your vision by 25%. Vitamins C and E, the antioxidants lutein and zeaxanthin, as well as the minerals zinc and copper, are all present in the composition.
Your doctor could advise you to undertake dietary and lifestyle modifications, such as quitting smoking. They could advise adding additional vegetables, fruits, and fatty seafood like salmon and mackerel to your diet. To reduce your blood cholesterol, you could be told to consume less red meat.
Early detection
If you have drusen, your doctor may advise you to monitor your eyesight at home using the Amsler Grid test. Early detection of wet macular degeneration may allow your doctor to administer injections of medicine to stabilize or restore your eyesight. You can reduce vision loss and delay consequences with early diagnosis.
FAQ’s
Can Drusen be serious?
Some people may not have issues with little drusen, but bigger drusen can raise your chance of developing age-related macular degeneration (AMD).
What does the term “macular drusen” mean?
Macular drusen, which are yellow deposits, form between the choroid layer, a layer of blood vessels that feeds the macula, and the retinal pigment epithelium.
They are found in the macular area of the retina.
Can drusen go away?
Drusen have a dynamic character and are a significant risk factor for neovascular age-related macular degeneration (AMD). They can grow, create new ones, or even go away over time.
How quickly do drusen develop?
The transition from the early to the late stage might take up to ten years. Drusen cannot be seen on your own; it requires the knowledge and tools of an eye specialist to do so. During a normal eye checkup, your doctor could find drusen and might also ask you to have more frequent eye exams.
Do drusen always lead to macular degeneration?
Usually, drusen are discovered after a thorough eye examination. You don’t definitely have an eye disease just because you have a few minor drusen. The likelihood that you may develop or currently have age-related macular degeneration increases with the number of bigger drusen and obviously if they are in the macula.
Macular drusen are how prevalent?
In 77.6% of eyes, the drusen were found in the macular area, and in 22.4% of eyes, they were extramacular. Conclusions: According to these statistics, drusen are frequently found in people between the ages of 20 and 49, however, they are typically considerably less than 63 um in size and tend to be smaller yet.
Do drusen result from excessive cholesterol?
It is well known that drusen, or cholesterol deposits, form in the eyes. The research, which was published in the journal Cell Metabolism, demonstrates that aging causes macrophages, which are big cells, to become less effective at their job of removing cholesterol from the eye.
Are drusen always harmful?
Drusen are mostly harmless when they are few and tiny. The likelihood of developing dry age-related macular degeneration rises as the quantity or size of these deposits increases. The most common cause of visual loss is age-related macular degeneration or AMD.
Do statins reduce macular degeneration?
Utilizing statins was proven to be protective against early and exudative AMD in a recent investigation.