What is uveitic glaucoma?
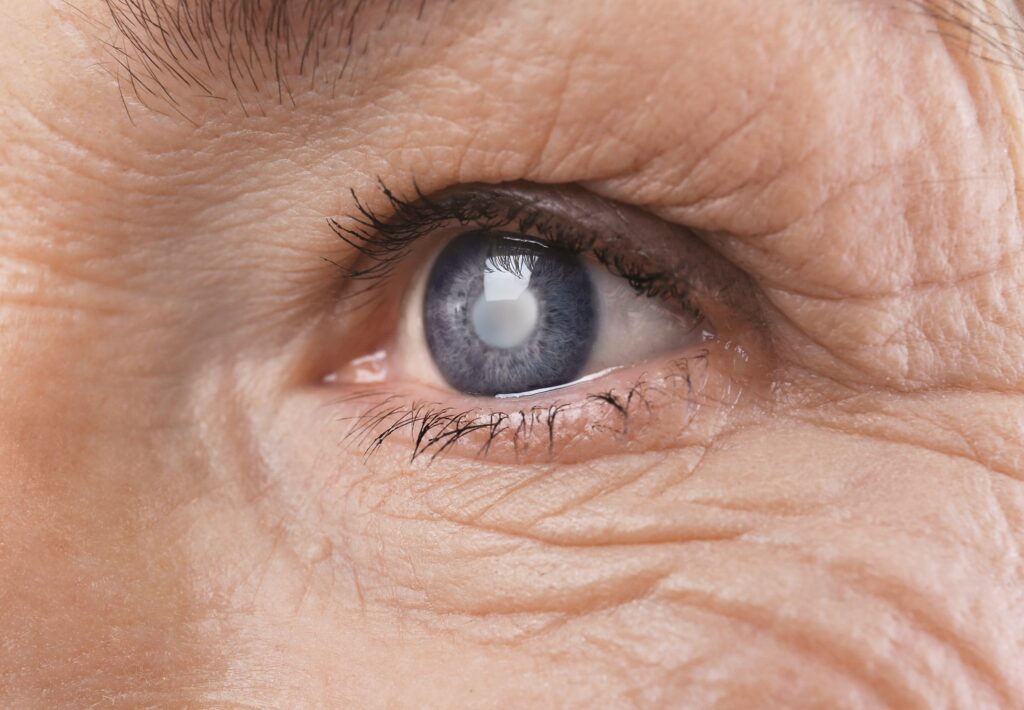
A form of glaucoma that develops as a side effect of uveitis is referred to as uveitic glaucoma, also known as uveitis-associated glaucoma or inflammatory glaucoma. The central layer of the eye, the uvea, which contains the iris, ciliary body, and choroid, is affected by the inflammatory disorder known as uveitis.
Inflammation brought on by uveitis can obstruct the eye’s regular fluid flow, raising intraocular pressure (IOP). Glaucoma may develop as a result of optic nerve damage brought on by elevated IOP. Therefore, uveitic glaucoma is characterized by both the uveitis’s inflammation and glaucoma’s increased intraocular pressure.
Although the precise mechanisms causing uveitic glaucoma are not well known, it is thought to involve a number of variables. The trabecular meshwork, which drains aqueous humor from the eye, can become clogged or destroyed as a result of inflammation inside the eye. This might prevent fluid from draining and raise IOP.
Eye pain, redness, impaired vision, sensitivity to light, and a rise in floaters are a few signs of uveitic glaucoma. It can result in loss of vision that is permanent if untreated.
In order to effectively treat uveitic glaucoma, it is often necessary to treat both the uveitis and the increased intraocular pressure. To manage the uveitis and lessen the inflammation, this may entail taking topical or systemic anti-inflammatory drugs. Additionally, a number of techniques, including topical or oral glaucoma drugs, laser therapy (such as selective laser trabeculoplasty or laser peripheral iridotomy), or in extreme circumstances, surgical interventions such trabeculectomy or glaucoma drainage devices, can be utilized to lower IOP.
To control the condition and lower their risk of developing uveitic glaucoma, people with uveitis should have regular eye exams and work closely with an ophthalmologist or uveitis specialist.
What are the common conditions associated with Uveitic Glaucoma?
Different underlying disorders that produce uveitis may be linked to uveitic glaucoma, which develops as a subsequent consequence. Uveitic glaucoma is often accompanied by the following conditions:
The most prevalent type of uveitis, anterior uveitis, causes inflammation largely in the iris and ciliary body at the front of the eye. Uveitic glaucoma frequently coexists with anterior uveitis.
Intermediate Uveitis: The vitreous gel and the center portion of the eye are both affected by intermediate uveitis. Uveitic glaucoma can also result from it, albeit it is less prevalent than anterior uveitis.
Posterior Uveitis
Posterior uveitis affects the choroid and retina in the back of the eye. Compared to anterior and intermediate uveitis, it is less frequently linked to uveitic glaucoma, but it can still happen.
Panuveitis
Panuveitis is an inflammation that affects the front, middle, and rear portions of the eye as well as all layers of the uvea. Uveitic glaucoma risk is considerably increased by panuveitis.
Uveitis
Uveitis can also be linked to a number of systemic inflammatory diseases, including Behçet’s disease, juvenile idiopathic arthritis, sarcoidosis, ankylosing spondylitis, and rheumatoid arthritis. Uveitic glaucoma can be brought on by certain systemic conditions.
Uveitis and consequent uveitic glaucoma can be caused by infections like the herpes simplex virus, varicella-zoster virus, toxoplasmosis, syphilis, TB, and others.
Not all cases of uveitis will result in the development of glaucoma, despite the fact that it is a common risk factor for the disease. Uveitis sufferers should, therefore, be regularly watched for the potential onset of glaucoma as early detection and treatment are essential for maintaining vision.
Uveitic Glaucoma Causes
Sometimes, uveitic glaucoma might be a symptom or an early indicator of a systemic illness. The condition uveitis itself, which can cause uveitic glaucoma, is frequently linked to other systemic diseases. Therefore, it is crucial for medical personnel to examine the patient for any underlying systemic disorders that may be causing the eye problem when uveitic glaucoma is discovered.
Uveitic glaucoma may occasionally be the initial symptom of a systemic disease, particularly if the patient hasn’t previously displayed any signs or symptoms of the underlying disorder. Uveitis and glaucoma can trigger additional research to find and properly treat the underlying systemic condition.
The following are typical systemic conditions linked to uveitis and uveitic glaucoma:
- Rheumatoid arthritis
- Ankylosing spondylitis
- Juvenile idiopathic arthritis
- Behçet’s disease
- Sarcoidosis
- Inflammatory bowel disease (such as Crohn’s disease and ulcerative colitis)
- Psoriasis
- Systemic lupus erythematosus
- Vasculitis
To ascertain whether any underlying systemic problems are present, it is important for those who have been diagnosed with uveitic glaucoma to have a complete evaluation by a healthcare specialist. To properly diagnose and treat the systemic condition, this may entail additional medical examinations, laboratory tests, and consultation with other specialists, including rheumatologists or internists.
Is there a common biomarker or test for these conditions?
Clinical assessment, medical history, and specific testing are frequently combined to make the diagnosis of underlying systemic disorders linked to uveitis and uveitic glaucoma. There are a number of studies that can be carried out to help with the diagnosis even though there isn’t a single universal biomarker or test that can conclusively identify all systemic disorders associated with uveitis. In the assessment of these conditions, the following frequent tests and biomarkers are employed:
Laboratory Tests
Blood tests can be run to look for particular inflammatory markers and antibodies linked to a number of systemic disorders. Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, antinuclear antibodies (ANA), human leukocyte antigen (HLA)-B27, and other markers are examples. The suspected systemic disease is determined by the clinical presentation and other variables, and the tests are chosen accordingly.
Imaging Studies
To assess the joints, spine, lungs, or other organs affected by systemic disorders, imaging techniques like X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans can be employed. These imaging tests can be used to spot indications of organ involvement, joint damage, or inflammation.
Ophthalmologic Examination
Diagnosing uveitis and uveitic glaucoma requires a comprehensive eye examination by an ophthalmologist. Examining the eye’s anterior and posterior segments, evaluating intraocular pressure, and determining the extent and location of uveitis are all possible inspection procedures. This assessment can assist direct follow-up inquiries and identify the best course of action.
Rheumatologic Consultation
Referral to a rheumatologist may be required when a systemic condition is suspected. Rheumatologists are experts in identifying and treating illnesses that cause systemic inflammation. To make a diagnosis, they can carry out a thorough evaluation and take into account the patient’s symptoms, medical history, physical examination findings, and the outcomes of laboratory testing.
It is imperative to remember that the diagnosis of systemic disorders linked to uveitis and uveitic glaucoma is frequently difficult and necessitates a multidisciplinary approach. Collaboration between rheumatologists, internists, ophthalmologists, and other specialists is essential for making an accurate diagnosis and starting the right course of treatment.
How is Uveitic Glaucoma diagnosed?
A combination of clinical assessment, examination, and specialist testing is used to determine the diagnosis of uveitic glaucoma. Usually, a glaucoma expert or an ophthalmologist must be involved. The following procedures may be used in the diagnosis of uveitic glaucoma:
Medical History and Symptoms
The doctor will begin by gathering all relevant information about your health, including any symptoms you may be feeling. Your eye health, prior uveitis episodes, systemic problems, medications, and family history of eye diseases will all be questioned.
Eye Exam
To evaluate the structures of the eye, a thorough eye exam will be performed. This could entail measuring visual acuity and evaluating the cornea, iris, and lens in the anterior segment of the eye, as well as the retina and optic nerve in the posterior region. The doctor will also use a tonometer to assess the intraocular pressure (IOP).
Gonioscopy
This examination measures the angle at which the eye drains. It assists in identifying any trabecular meshwork anomalies or obstructions that can affect fluid outflow and result in increased IOP.
Visual Field Testing
Visual Field Testing is done to gauge peripheral vision. It can identify any glaucoma-related anomalies or visual field impairments. This test aids in determining the degree of vision loss and tracking its progression over time.
Evaluation of the Optic Nerve
Ophthalmoscopy or other imaging methods, such as optical coherence tomography (OCT), will be used to look at the optic nerve. These techniques aid in assessing the integrity and health of the optic nerve, which can be impacted by glaucoma.
Intraocular pressure (IOP) measurement
Glaucoma is characterized by elevated IOP. Tonometry may be used by the doctor to calculate IOP. To evaluate the variability of IOP, many measurements may be done at various intervals.
Evaluation of Uveitis
The ophthalmologist or optometrist will assess the presence and symptoms of uveitis. This may entail evaluating the presence of inflammation, establishing the kind of uveitis involved (panuveitis, anterior, intermediate, or posterior), and identifying any accompanying symptoms.
Additional Tests
Additional tests may be requested depending on the circumstances of each case to help with diagnosis and treatment planning. These could consist of blood tests, imaging investigations (such as OCT or ultrasound), and specialized tests to find certain antibodies or biomarkers linked to uveitis or underlying systemic disorders.
Depending on the clinical presentation, severity, and suspected underlying reasons, the specific diagnostic technique may change. For an accurate diagnosis and effective treatment of uveitic glaucoma, speak with an eye care specialist or professional.
Is uveitic glaucoma open or closed angle?
Depending on the underlying processes, uveitic glaucoma can show as either open-angle or closed-angle glaucoma.
The more prevalent type of uveitic glaucoma is open-angle glaucoma. Elevated intraocular pressure (IOP) results from greater resistance to aqueous humor exiting the trabecular meshwork, which causes it to happen. The uveitis-related inflammation may alter the trabecular meshwork’s structural integrity or obstruct normal fluid drainage from the eye. As a result, the IOP rises and open-angle uveitic glaucoma develops.
Closed-Angle Uveitic Glaucoma
This type of uveitic glaucoma, also known as angle-closure glaucoma, is rather uncommon. It happens when the drainage angle in the eye becomes suddenly or gradually blocked, leading to an abrupt rise in intraocular pressure. Inflammatory debris, peripheral anterior synechiae (adhesions between the iris and cornea), or iris edema can all contribute to the obstruction. This prevents aqueous humor from flowing and results in a closed-angle glaucoma appearance.
The contrast between open-angle and closed-angle glaucoma is significant because it relates to the particular mechanism of outflow restriction. Whether it is open-angle or closed-angle glaucoma, the underlying inflammation and related changes within the eye contribute to the development of high intraocular pressure. To stop additional harm to the optic nerve and preserve vision, the treatment strategy for uveitic glaucoma tries to address the underlying inflammation and control the raised intraocular pressure.
Summary
Uveitic glaucoma patients should contact their eye doctor for regular follow-up appointments in order to track the condition’s development. Regular eye exams, intraocular pressure readings, visual field tests, and optic nerve health checks are all part of this. The severity of the problem and how well treatment is working will determine how frequently you need to return.
Maintaining open lines of communication with the ophthalmologist and any other healthcare professionals engaged in the treatment of the underlying systemic illness is crucial. Talk with them about any concerns or questions you may have, as well as any changes in your symptoms or any unwanted effects from your medicine.
FAQ’s
Can uveitis glaucoma be cured?
It’s important to identify and treat the etiology of uveitis. After treating the increased IOP, it is important to check for steroid-induced ocular hypertension. To fully treat uveitis glaucoma, medical and surgical treatment options are available.
Can you have uveitis and not go blind?
Although it is rare, problems from uveitis can occasionally include vision loss.
How is glaucoma uveitis managed?
Controlling the inflammation is the aim of uveitis treatment. Steroid usage is the most typical method of treating uveitis, with steroid eye drops serving as the most typical first line of defense. Steroid injections in or near the eye and/or oral steroids in pill form are other therapy options.