Hearing the term corneal dystrophy might sound scary, but it’s okay to have questions. Simply put, corneal dystrophy is a group of genetic eye conditions that affect the cornea, the clear front part of your eye. These conditions aren’t caused by anything you did; they’re inherited, meaning they run in families.
Corneal dystrophy is not very common. It affects less than 1% of people, and research suggests that around 1 in every 1,500 to 2,000 people worldwide experience this condition.
From my experience helping people with their vision, I’ve learned that simple, easy-to-understand information can make a big difference. My goal is to explain corneal dystrophy in a calm and clear way. We’ll cover what it is, the types of corneal dystrophy, and the many treatments that can help. It’s also important to know that while these conditions are progressive, they usually develop very slowly. With the right care, most people can keep good vision throughout their lives.
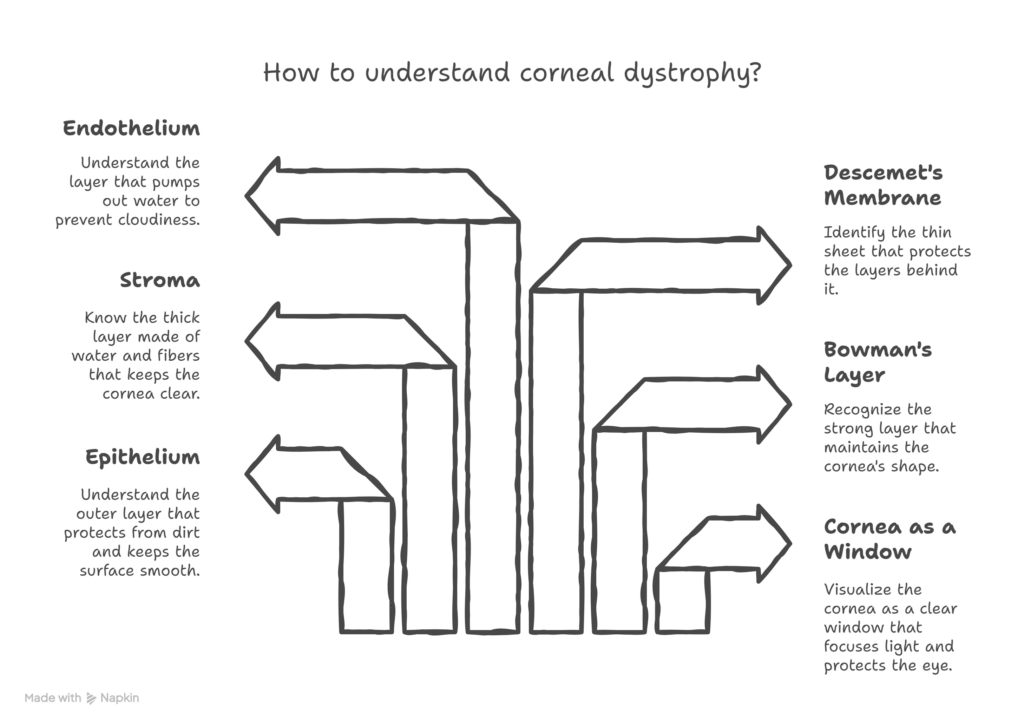
Understanding the Cornea
To understand corneal dystrophy, it helps to first know about the cornea. Think of your cornea as the clear front window of your eye. It helps you see clearly by focusing light. It also protects your eyes from things like dust and germs.
Your cornea needs to be clear for you to have sharp vision. It’s very thin but has five different layers. Each layer has a job to keep your cornea healthy.
- Epithelium: This is the outside layer. It protects your eye from dirt and keeps its surface smooth.
- Bowman’s Layer: A strong layer right behind the epithelium that helps give the cornea its shape.
- Stroma: This is the thickest layer. It’s made of water and fibers that keep the cornea clear.
- Descemet’s Membrane: A thin sheet that protects the layers behind it.
- Endothelium: This is the very last layer. Its important job is to pump out extra water to keep the cornea from getting cloudy.
If any of these layers don’t work the right way, it can make your cornea cloudy and affect your vision.
What Is Corneal Dystrophy?
Corneal dystrophy is a genetic, inherited, and usually bilateral condition that affects the clarity and structure of the cornea. It is non-inflammatory, and its changes occur over time due to DNA mutations. These mutations cause material to build up in the cornea, slowly impacting vision.
- Key Features of Corneal Dystrophy
- Hereditary/Genetic: Caused by gene mutations that affect corneal proteins.
- Bilateral: Typically impacts both eyes, though severity can vary between them.
- Non-inflammatory: Clouding happens due to deposits, not infection or inflammation.
- Progressive: Develops gradually over many years.
- Broad Term: Includes over 20 types that affect different corneal layers.
- How Genetics Plays a Role?
DNA mutations change how corneal proteins form or clear, causing deposits of proteins, lipids, or amyloids within specific corneal layers. These inherited changes can follow different patterns:
- Autosomal dominant: Most common inheritance type.
- Autosomal recessive: Seen in certain forms, like macular dystrophy.
- Complex inheritance: Found in some less common types.
- Core Characteristics
- Corneal dystrophies are not caused by screen use, lifestyle, or environmental factors.
- Both eyes are generally affected, and the condition progresses slowly over time.
- Symptoms vary, but the process is non-inflammatory.
3. How It Differs From Other Corneal Conditions?
| Feature | Corneal Dystrophy | Corneal Degeneration | Keratoconus |
| Main Cause | Genetic; inherited mutations | Age-related or chronic wear/tear | Biomechanical weakness; not genetic in most cases |
| Onset | Early to mid-life | Later in life | Teen to early adulthood |
| Inflammation | Non-inflammatory | Typically non-inflammatory | Non-inflammatory |
| Progression | Slow and predictable | Varies by type | Progressive thinning and steepening |
| What Happens? | Material builds up in the corneal layers | Tissue degenerates over time | The cornea thins and bulges outward |
| Symptoms | Blurred vision, glare, erosions | Dryness, reduced clarity | Distorted vision, changing prescriptions |
| Laterality | Usually affects both eyes | Can be unilateral or bilateral | Often bilateral but uneven |
| Treatment | Depends on the layer affected, may include drops or surgery | Manage dryness, address causes | Cross-linking, specialty lenses, and potential transplant |
- Emotional Perspective
Receiving a corneal dystrophy diagnosis can feel overwhelming, but it’s important to know that many people maintain good vision with regular monitoring and appropriate treatment. Understanding the condition empowers you to manage it confidently and focus on solutions that improve your quality of life. Everyone’s condition is different, most of my patients with corneal dystrophies do just fine, it is a rare situation that someone might need a transplant.
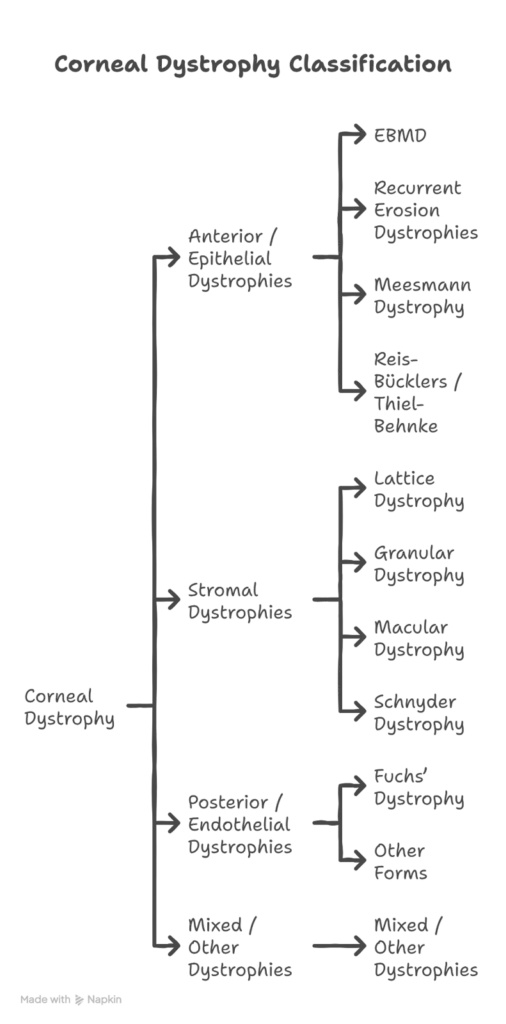
Types of Corneal Dystrophy by Layer
Corneal dystrophies are categorized based on the layer of the cornea they affect. The IC3D system groups them into four main types:
- Anterior / Epithelial Dystrophies
These affect the outer layers of the cornea, such as the epithelium and Bowman’s layer, which can lead to surface irregularities and recurring erosions. Symptoms often include mild vision changes and discomfort, especially in the morning. I have many patients with these conditions, most of the time they are just slightly annoying due to discomfort. Most still see fine.
- EBMD (Map-dot-fingerprint): A common condition that causes fluctuating vision and morning eye pain.
- Recurrent Erosion Dystrophies: The surface layer does not adhere well, leading to sharp pain upon waking.
- Meesmann Dystrophy: Small epithelial cysts appear from childhood and cause mild irritation.
- Reis-Bücklers / Thiel-Behnke: These conditions create surface roughness and glare. Sometimes, specialized treatments like PTK are needed.
- Stromal Dystrophies
These affect the middle layer (stroma), leading to protein or lipid deposits and gradual clouding of the cornea. These conditions aren’t usually uncomfortable but can cause somewhat worse vision.
- Lattice Dystrophy: Shows as lines of amyloid deposits; severe cases may require a transplant.
- Granular Dystrophy: Small crumb-like spots form in the stroma; Type II may also show lattice-like features.
- Macular Dystrophy: A more severe type, causing diffuse cloudiness; often inherited recessively.
- Schnyder Dystrophy: Cholesterol crystals build up in the cornea. Lipid levels should also be monitored.
- Posterior / Endothelial Dystrophies
These involve the inner layers like Descemet’s membrane and endothelium, leading to corneal swelling (edema) and blurred vision. These conditions can lead to more severe complications.
- Fuchs’ Dystrophy: The most common type, starting with blurry vision in the morning and progressing to chronic haze. Advanced cases may require transplants like DSEK or DMEK.
- Other Forms: PPCD is generally mild, while CHED leads to childhood cloudiness.
- Mixed / Other Dystrophies
These dystrophies impact multiple layers of the cornea. Classification is evolving as research advances, and treatment focuses on the severity of symptoms.
Each of these types requires tailored management to minimize symptoms and preserve vision as much as possible.
Symptoms & Warning Signs
Corneal dystrophies usually progress slowly over many years, and early on, most people don’t notice any symptoms. The signs can differ depending on the type and severity of the condition.
- Common Symptoms Across Types
- Visual Symptoms
People often experience gradually blurry or cloudy vision, which can feel like looking through a foggy or dirty window. Glare, halos, trouble seeing at night, and reduced contrast are also common. Some may find their glasses prescription needs frequent changes as the cornea becomes less clear. - Physical Symptoms
Pain, especially in the morning, is a common sign. Other symptoms include a feeling of something in the eye, tearing, sensitivity to light, and occasional redness. These occur due to irregularities or swelling on the cornea’s surface. - Timing Patterns
Symptoms are often worse in the mornings, especially with conditions like Fuchs’ dystrophy or recurrent corneal erosions. Vision may change throughout the day as the cornea adjusts in thickness or moisture. However, many people don’t have symptoms in the early stages and are diagnosed during regular eye checkups.
2. Type-Specific Patterns
- Epithelial / Surface Dystrophies – “Painful Mornings”
These types often cause painful episodes when waking up, because the eyelid can stick to the corneal surface. Between episodes, vision may be normal, but the pain during these events can be sharp and significant. - Stromal Dystrophies – “Cloudy Over Time”
These conditions lead to a gradual buildup of haze in the cornea, causing vision to worsen slowly. Specific patterns, like streaks in lattice dystrophy or white spots in granular dystrophy, may be noticeable. - Endothelial / Fuchs’ Dystrophy – “Morning Blur + Swelling.”
Early in this condition, vision is often blurry in the morning but improves as the day goes on, as the cornea naturally dries out. Later stages bring constant swelling, blurry vision, and sometimes painful blisters on the eye’s surface.
When to See a Doctor?
You should have a routine eye exam if you notice any gradual changes in your vision, have a family history of corneal dystrophy, or start experiencing glare or morning blurriness. Many of my patients just feel like they have chronic dry eyes, you should still get checked.
Seek immediate medical care if you experience:
- A sudden, significant loss of vision.
- Severe eye pain that does not go away.
- An injury to your eye.
- Signs of an infection, such as pus-like discharge or extreme redness.
- Routine Exam Needed If:
- You notice a gradual blurring of your vision or have trouble with glare, especially at night.
- You have a family history of corneal dystrophy.
- Your vision is blurry in the morning but clears later in the day.
- You experience persistent halos or glare around lights.
- New or ongoing symptoms develop, like irritation or tearing.
Early evaluation is key to maintaining comfort and protecting your long-term vision. Reporting symptoms early is a proactive step, not a cause for alarm.
The Causes: It’s All in the Genes
It is very important to understand that corneal dystrophies are caused by genetics. You did nothing to cause this condition, and you could not have prevented it.
Specific genes contain the instructions for building the proteins that keep the cornea clear and healthy. In corneal dystrophy, there is a “mistake” or mutation in one of these genes. This leads to the production of faulty proteins or the buildup of abnormal materials in the cornea.
The gene most often involved is called TGFBI. Mutations in this single gene can cause several different stromal dystrophies, including Lattice and Granular. For Fuchs’ dystrophy, changes in genes like TCF4 are often responsible.
- How Corneal Dystrophy is Inherited?
There are a few ways these genetic changes can be passed down in families:
- Autosomal Dominant:
This is the most common pattern. It means you only need to inherit one copy of the mutated gene from one parent to have the condition. If a parent has it, each child has a 50% chance of inheriting it. Most dystrophies, including Fuchs’, Lattice, and Granular, follow this pattern. - Autosomal Recessive:
This pattern is less common. It means you must inherit two copies of the mutated gene from each parent to have the condition. The parents are usually “carriers” who have one copy of the gene but no symptoms. Macular dystrophy is inherited this way. - Sporadic Cases:
Sometimes, a new mutation occurs in a person with no family history of the condition. They can still pass this gene on to their children.
It’s also important to know that just because you have the gene doesn’t mean you will have severe symptoms. The severity can vary greatly, even among family members with the same mutation. This is why genetic counseling can be helpful for families.
2. Risk Factors
Certain factors can increase the likelihood of developing macular dystrophy. Let’s look at them one by one.
- Family History: This is the most significant risk factor. Since most corneal dystrophies are genetic, having a family member with the condition increases your risk.
- Age: Many types of corneal dystrophy begin to show symptoms after age 40, though some can appear much earlier in life.
- Gender: Some dystrophies are more common in one gender over another. For instance, Fuchs’ dystrophy affects women more often than men.
- Ethnicity: The prevalence of certain dystrophies can vary among different ethnic groups or people from specific geographic regions.
It is also reassuring to know what does not cause macular dystrophy. The condition is not caused by lifestyle factors such as screen time, diet, reading too much, eye infections, injuries, or wearing contact lenses.
While you cannot prevent inheriting a gene, you can take positive steps. Regular eye exams and working with your doctor to manage the condition can help protect your vision for the long term. Genetic counseling can also provide clarity and help you and your family plan for the future.
Its important to know that even though you may be diagnosed with a corneal dystrophy the majority of people won’t have any problems from it, so don’t get to worked up about it to begin with.
Diagnosis Process
Corneal dystrophy is often discovered unexpectedly during routine eye exams or when symptoms begin to appear. The tests to diagnose this condition are simple, painless, and typically done in a clinic.
When Dystrophy Is Discovered?
- Incidental Finding (No Symptoms):
During routine check-ups, doctors may notice tiny deposits or a hazy appearance in the cornea. If there are no symptoms, treatment might not be needed, but regular monitoring can provide reassurance. - Symptomatic Presentation:
People may seek care due to symptoms like blurry vision, eye pain, morning erosions, glare/halos, or because of a family history of the condition. These symptoms help guide doctors in testing and creating a management plan.
How a Diagnosis is Made?
A diagnosis of corneal dystrophy is often made during a routine eye exam, sometimes even before you have any symptoms. Your eye doctor will use several painless tests.
- Slit-Lamp Exam: This is the most important tool. A slit lamp is a special microscope that allows your doctor to look at your cornea in great detail. They can see the specific patterns of deposits, identify which layer is affected, and check for any swelling.
- Corneal Pachymetry: This quick, painless test uses ultrasound to measure the thickness of your cornea. A thicker-than-normal cornea is a sign of swelling (edema), which is common in Fuchs’ dystrophy.
- Specular Microscopy: This test takes a photograph of the endothelial cells on the back layer of your cornea. It allows your doctor to count the cells. In Fuchs’ dystrophy, the cell count is lower than normal.
- Genetic Testing: A blood test or cheek swab can be used to identify the specific gene mutation. This is not always necessary for diagnosis, as the slit-lamp exam is often enough. However, it can be useful for confirming a diagnosis or for family planning.
A Guide to Treatment Options
The treatment for corneal dystrophy depends entirely on your symptoms and the severity of your condition. If you have no symptoms, the best approach is often just regular monitoring. For those with symptoms, the goal is to improve vision and provide comfort.
- Conservative and Medical Treatments (For Mild to Moderate Symptoms)
- Lubricating Eye Drops and Ointments:
Artificial tears can help with feelings of dryness or grittiness. A thick ointment at bedtime can prevent the eyelid from sticking to the cornea, which is very helpful for people with recurrent erosions. - Hypertonic Saline (Salt) Drops or Ointment:
For people with early Fuchs’ dystrophy, these special drops (5% sodium chloride) can help pull fluid out of the cornea, reducing swelling and temporarily clearing up morning blurriness. - The Hair Dryer Technique:
Some people with Fuchs’ find it helpful to hold a hair dryer at arm’s length and blow cool or warm air toward their face for a few minutes in the morning. This can help evaporate excess fluid from the cornea and clear up vision faster. - Bandage Contact Lenses:
For painful recurrent erosions, a doctor can place a special soft contact lens on the eye. It acts like a bandage, protecting the healing surface and relieving pain. - Phototherapeutic Keratectomy (PTK):
This is a laser procedure used for some anterior dystrophies. The laser removes a very thin layer from the surface of the cornea, smoothing out irregularities and removing cloudy deposits.
- Surgical Treatment: Corneal Transplantation
When vision becomes severely affected, and other treatments are not enough, a corneal transplant may be recommended. For decades, the only option was a full-thickness transplant (penetrating keratoplasty, or PK). Today, surgeons can often replace only the diseased layers of the cornea, which leads to faster recovery and better outcomes.
Modern corneal transplant surgery is incredibly successful. The type of transplant depends on which layer of the cornea is affected.
- For Stromal Dystrophies (like Lattice or Granular): A surgeon might perform a Deep Anterior Lamellar Keratoplasty (DALK). This procedure replaces the front and middle layers of the cornea but leaves your own healthy endothelium in place. This greatly reduces the risk of the transplant being rejected by your body.
- For Fuchs’ Dystrophy: The standard of care today is a type of partial-thickness transplant that replaces only the back layer of the cornea.
- DSEK (Descemet’s Stripping Endothelial Keratoplasty): The surgeon removes the diseased endothelium and replaces it with a thin piece of donor tissue.
- DMEK (Descemet’s Membrane Endothelial Keratoplasty): This is an even more advanced procedure where only the Descemet’s membrane and endothelium layer, thinner than a human hair, are replaced. DMEK offers the fastest recovery and sharpest possible vision.
After a DMEK or DSEK procedure, you will need to lie flat on your back for a day or two to allow an air bubble to press the new tissue into place. Vision recovery is much faster than with a full transplant, often improving within weeks or even days.
Living Well with Corneal Dystrophy
Receiving a diagnosis is one thing; learning to live with it day to day is another. The good news is that there are many tools and strategies that can help you maintain your independence and quality of life.
- Vision Aids and Assistive Technology
Managing symptoms like glare and reduced clarity can make a huge difference.
- For Glare and Light Sensitivity:
- Polarized sunglasses are excellent for reducing glare outdoors.
- Anti-reflective coating on your regular glasses can help with indoor glare and nighttime driving.
- Some people find that lightly tinted indoor glasses (like an FL-41 tint) make them more comfortable under fluorescent lights.
- For Blurry Vision or Difficulty Reading:
- Stronger reading glasses are a simple first step.
- Magnifiers come in all shapes and sizes, from small handheld ones to larger electronic video magnifiers (CCTVs) that can enlarge text onto a screen.
- Good lighting is essential. A bright, focused task light directed onto your book or project can make a world of difference.
- Technology to Help:
- Modern smartphones and computers have wonderful accessibility features built in. You can increase text size, choose high-contrast modes, and use text-to-speech functions to have emails or articles read aloud to you.
A low vision specialist can help you find the right tools for your specific needs. These aids don’t cure the condition, but they can help you work around the vision loss in very practical ways.
2. Lifestyle and Home Adaptations
Simple Changes at Home
Simple adjustments at home can make a big difference in safety and independence.
- Keep things organized: Store essential items in the same place so they’re easy to find.
- Use labels: Apply bold or tactile labels to appliances and containers.
- Improve lighting: Brighten hallways and declutter walkways to prevent trips.
- Add contrast: Use high-contrast colors for light switches, stairs, and kitchen tools to make them more visible.
3. Reading and Daily Tasks
The right tools can make reading and other tasks much easier.
- Use bright, focused lighting on your book or project.
- Use technology: Increase the font size on your devices or use text-to-speech functions to have articles read aloud.
- Listen instead: Switch to audiobooks or podcasts if reading becomes tiring.
4. Emotional Support
Taking care of your emotional well-being is an important part of adjusting to vision loss.
- Talk to loved ones: Share your experiences with family and friends so they can better understand how to support you.
- Find community: Join a support group to connect with others who share similar experiences.
- Stay positive: Focus on what you can do, not what you can’t. Staying socially active and seeking counseling if needed can help you maintain a positive outlook.
5. Support at Work
Simple accommodations can help you stay productive and comfortable at work.
- Use helpful tools: Screen magnifiers, large monitors, and better lighting can make tasks more manageable.
- Ask for flexibility: Your employer may be able to offer a flexible schedule or modify certain tasks.
- Know your rights: Disability laws protect your right to fair accommodations in the workplace.
6. Driving Considerations
- Recognize changes: Driving is a big part of independence, which can make it hard to consider stopping. But it’s important to put safety first for yourself and others on the road.
- Acknowledge warning signs: If you start having trouble with glare, reading road signs, or driving at night, it’s a clear signal that it’s time to think about your driving habits.
- Seek advice: Talk to your eye doctor and your family about your concerns. They can offer guidance and help you make a safe and informed decision.
7. Planning for Progression
Good planning reduces stress and helps you prepare for vision changes.
- Stay proactive with:
- Regular check-ups
- Early treatment discussions
- Financial planning
- A strong support network
- Prognoses vary by dystrophy type, but:
- Early care improves outcomes
- Advanced treatments and technology can help
- With proper care and support, many maintain useful vision for years.
8. Quality of Life Outlook
With proper care, many people with corneal dystrophies continue leading independent lives. Reading, working, and managing daily tasks are possible with the help of vision aids, magnifiers, and good lighting. Some may choose to limit night driving, but most routines remain unaffected. Transplants have a high success rate, with over 90% graft clarity, and vision often stabilizes within months after surgery. With ongoing advancements in treatments, support systems, and tools, maintaining a good quality of life is achievable and hopeful.
9. Prevention and Family Screening
Corneal dystrophies are genetic, so early detection and regular monitoring are key. Family members may benefit from screening to spot changes early, allowing for better outcomes and planning.
Can Corneal Dystrophy Be Prevented?
No, corneal dystrophy cannot be prevented because it is caused by genetic changes in your DNA. It is not linked to lifestyle, diet, screen use, reading habits, or overall health. However, practicing healthy eye care habits, such as wearing UV protection, managing medical conditions like diabetes, using safety eyewear, and avoiding smoking, can help maintain general eye health. While these habits cannot stop the genetic condition, they support overall eye wellness.
Early detection is important because it allows for:
- Careful monitoring over time.
- Treatment before symptoms become severe.
- Planning for work, driving, and finances.
- Screening family members if necessary.
- What You Can Control?
Here are steps you can take to manage corneal dystrophy effectively:
- Get regular eye exams, especially if you have a family history.
- Report symptoms like pain, blurry vision, or frequent erosions early.
- Follow treatment plans, including using prescribed eye drops or lenses and attending follow-up appointments.
- Use vision aids and adapt your lifestyle to maintain independence.
Research into gene therapy is ongoing and may provide new treatment options in the future.
- Family Screening for Corneal Dystrophies
- Recommended for first-degree relatives (parents, siblings, and children).
- Key tests: eye exam, slit lamp assessment, specular microscopy, and optional genetic testing.
- Benefits: early detection, monitoring baseline, and timely treatment.
- Supports families with inheritance risks and testing options through genetic counseling.
Research & Future Treatments
Current Research Areas
- Gene Therapy: Using tools like CRISPR to fix or silence faulty genes and prevent corneal dystrophies.
- Stem Cell Treatment: Replacing damaged corneal cells; promising trials underway.
- Drug Treatments: New medications aim to slow disease progression and reduce swelling.
- Advanced Surgery: Safer, faster procedures like DMEK improve recovery.
- Bioengineered Corneas: Lab-made corneas reduce reliance on donors.
- AI Tools: Early detection and personalized care through advanced screening.
What’s Ahead (5-10 Years)
- Gene therapies and personalized treatments
- New drugs to avoid transplants
- Better prediction tools
- Improved surgery access
Q&A About Corneal Dystrophy
Q1: Is corneal dystrophy the same as keratoconus?
No. Corneal dystrophy is a group of genetic eye conditions, while keratoconus is another condition where the cornea thins and bulges outward. Keratoconus mainly affects a specific layer of the cornea. There are over 20 types of corneal dystrophy. While both conditions can have genetic links, they are diagnosed and treated differently.
Q2: Will corneal dystrophy make me blind?
Complete blindness is very rare. Corneal dystrophy usually affects central vision but leaves side (peripheral) vision intact. Most people can keep good functional vision with treatment. Modern procedures, like corneal transplants, are highly successful and help keep vision stable.
Q3: Can I pass corneal dystrophy to my children?
Maybe. Some types are inherited through a dominant gene, which means there’s a 50% chance for each child, while others depend on both parents’ genes. Even if the gene is passed on, not everyone shows symptoms. Genetic counseling can help you understand the risks.
Q4: How quickly will my vision get worse?
Progression varies by type and person. For many, symptoms change slowly over many years, and some types remain mild. Regular eye exams can track changes, and treatments can slow or even stabilize progression. No one can predict the exact pace for you.
Q5: Should I avoid screens or UV light?
Screens do not make corneal dystrophy worse. Protecting your eyes from UV light is helpful for general eye health, but won’t stop dystrophy. To make screens easier to use, reduce glare, blink regularly, and take breaks.
Q6: Can surgery or LASIK worsen corneal dystrophy?
LASIK isn’t usually safe for corneal dystrophy since it may weaken the cornea. However, some procedures, like PTK or cross-linking (used for keratoconus), can help in certain cases. Your eye doctor will guide you on safe options.
Q7: Are there foods or supplements that help corneal dystrophy?
No specific foods or supplements treat corneal dystrophy. Eating a balanced diet and including omega-3 fatty acids can support overall eye health, but medical treatments are the main option for managing dystrophy.
Q8: How often should I get an eye exam?
If your condition is stable, yearly exams are usually enough. If symptoms worsen, exams every 3-6 months may be needed. After surgery or a procedure, follow-ups may be more frequent. Your doctor will advise you on the right schedule.
Q9: Is surgery for corneal dystrophy painful?
No, surgery isn’t painful because it’s done with anesthesia. You might feel mild discomfort afterward. Recovery time depends on the type of surgery; for example, DMEK heals faster than PK. Vision improves gradually, and most surgeries have great success rates.
Q10: Can I still wear contact lenses with corneal dystrophy?
It depends. Some types of dystrophy may make contact lenses uncomfortable or harmful. For conditions like keratoconus, special lenses are often needed. Your eye doctor can tell you what’s safe for your eyes.
Resources for Support
- Educational Materials
Trusted eye-health organizations and doctors provide clear guides on your condition. They offer articles, diagrams, and updates to help you understand treatments and research. - Patient Support
Connect with support groups or patient foundations. Programs like webinars and online communities can reduce stress, share advice, and help you feel less alone. - Genetics Information
Because corneal dystrophies often run in families, genetic testing and counseling can help you learn about risks and make informed choices. Ask your doctor about these options. - Low Vision Services
If your vision is reduced, low vision centers and specialists can help. They recommend tools like magnifiers, electronic readers, or better lighting to maintain your independence. They can also teach you how to use them effectively. - Affordable Care Assistance
Help is out there for covering costs. Community programs and foundations sometimes assist with glasses, surgeries, or transplant expenses. Ask about programs that fit your needs. - Clinical Trials
Research studies sometimes offer access to newer treatments. Talk to your doctor about finding trials that may be a good option for you.
Conclusion
Corneal dystrophies are manageable conditions, and with today’s diagnostic tools and treatment options, many people continue to live full, active, and independent lives. Early diagnosis, consistent follow-up care, and the right treatment plan can slow progression, reduce symptoms, and protect long-term vision. Whether your care plan includes monitoring, medication, surgical treatment, or visual rehabilitation, proactive eye care makes a meaningful difference.









