Imagine living in a world where seeing clearly is a daily struggle and every peek at the outside world is hampered by a birth defect. For those who have Primary Congenital Glaucoma (PCG), this is the reality. We will go deeply into the realm of PCG in this thorough guide, learning about what it is, how it affects the eyes, its causes, symptoms, diagnosis, available treatments, and much more. We’ll also talk about how Low Vision services can help people with this disability live better lives.
What is Primary Congenital Glaucoma?
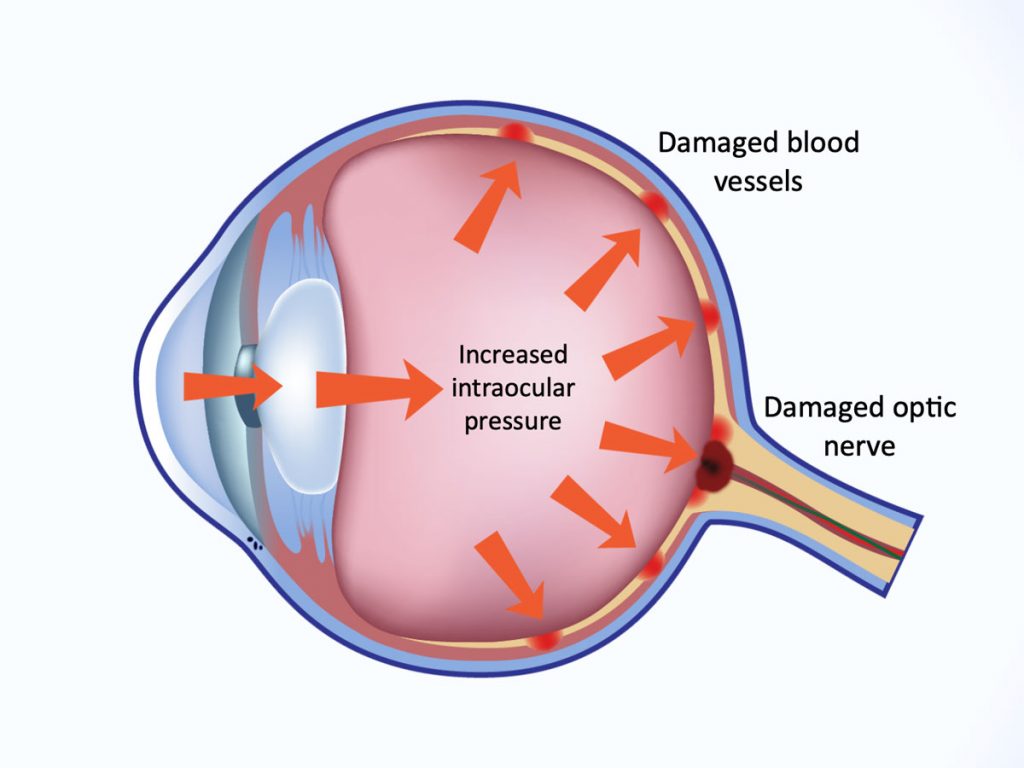
Congenital glaucoma, also known as primary congenital glaucoma (PCG), is a rare but serious eye condition that usually first appears in infancy or early childhood. If left untreated, this disorder, which is characterized by elevated intraocular pressure (IOP) as a result of irregularities in the eye’s drainage system, can damage the optic nerve and even cause vision loss.
How Does Primary Congenital Glaucoma Affect Your Eyes?
PCG primarily impacts the drainage system of the eye, which regulates intraocular pressure (IOP) in the eye. A breakdown in this drainage system causes fluid to accumulate in the eye, raising IOP. Irreversible vision loss may result from optic nerve injury brought on by elevated IOP.
What Causes Primary Congenital Glaucoma?
Although the precise origin of PCG is not always known, it is thought to be the result of a mix of hereditary and environmental factors. CYP1B1 and LTBP2 gene mutations, for example, have been linked to an increased risk of PCG. However, not every occurrence is connected to a particular genetic mutation, indicating that additional variables might possibly be involved.
Factors that Increase the Risk
Even though PCG is a rare disorder, some things can make you more likely to get it. These risk elements consist of:
Family history
People who have a history of PCG or other types of glaucoma may be at a higher risk.
Ethnicity
People of Middle Eastern or Romani heritage, for example, are more predisposed than other ethnic groupings.
Gender
PCG affects men more frequently than women.
Premature Birth
Infants who are born prematurely may be more likely to develop PCG.
Recognizing the Symptoms
For an early diagnosis and effective treatment of PCG, it is essential to recognize the early signs and symptoms. Typical signs include:
- Constant tears or moist eyes are examples of excessive crying.
- Photophobia: A fear of light.
- Eyelids closing involuntarily is referred to as blepharospasm.
- The affected eye may appear bigger than the unaffected one due to this condition.
- Hazy or cloudy cornea: As a result of fluid buildup and increasing pressure.
Primary Congenital Glaucoma Diagnosis
An eye doctor must perform a thorough examination to diagnose PCG. Typically, the diagnostic procedure entails:
Clinical Diagnosis
Physical Exam: The doctor will check the child’s eyes for indications of high IOP, such as enlarging corneas.
Tonometry: IOP is measured during this procedure. IOP elevation may be a sign of glaucoma.
Diagnostic Procedures
- Gonioscopy: This procedure uses a specialized lens to look at the eye’s drainage angle. In this location, PCG frequently exhibits a deformity.
- Ophthalmoscopy: This enables medical professionals to look for signs of injury to the optic nerve head.
Lab Tests
Genetic Testing: In some circumstances, genetic testing may be advised to find particular mutations connected to PCG.
Differential Diagnoses
It’s important to distinguish PCG from other eye disorders, such as pediatric cataracts or other types of glaucoma, that may present with identical symptoms.
Treatment Options
For PCG management and visual loss prevention, early diagnosis and intervention are essential. Depending on how severe the problem is, different treatment methods may be available.
Medical therapy is the main method of general treatment. In mild situations, eye drops or oral drugs may be advised to reduce intraocular pressure.
Surgical Intervention: In order to develop a new drainage conduit for the aqueous humor, surgery is frequently necessary. Trabeculectomy and goniotomy are the two primary surgical techniques employed.
Prostaglandin analogs, beta-blockers, and alpha agonists are typical drugs used to lower IOP in PCG patients’ medical therapy regimens.
Operative Intervention
Trabeculotomy: This operation involves making an aperture in the drainage system of the eye to enhance fluid outflow.
In order to assist fluid drainage, a small incision is made in the drainage angle during a goniotomy.
Surgical Follow-up
Patients will need to schedule routine follow-up appointments after surgery in order to track IOP and guarantee the procedure’s success. In some circumstances, more procedures may be required.
Potential Complications
While managing PCG and maintaining eyesight are the main objectives of treatment, problems can still occur. These may consist of:
- High IOP and corneal injury cause scarring on the cornea.
- If not treated right away, amblyopia (lazy eye) can cause reduced vision in the affected eye.
- Vision loss brought on by glaucoma: in severe cases or if treatment is postponed.
Prognosis Depending on the severity of the ailment and how quickly it is treated, PCG’s prognosis can change. Many people with PCG can preserve good vision and lead normal lives with early diagnosis and effective management. Regular follow-up care is necessary to check for potential problems, though.
Could There Be Complications?
Yes, problems might develop if PCG is not properly managed. It’s critical to realize that PCG is a chronic illness that necessitates constant attention and observation. The risk of problems can be reduced by adhering to the recommended course of therapy from an eye doctor.
Difference between Primary Open-Angle Glaucoma and Primary Congenital Glaucoma
Primary Open-Angle Glaucoma (POAG) and Primary Congenital Glaucoma (PCG) are two separate forms of glaucoma that vary significantly in a number of important ways. Here is a contrast between the two situations:
Age of Onset:
- PCG: In infancy or the early years of life, PCG is commonly diagnosed. It exists from birth or manifests itself during the first few years of life.
- POAG: POAG often appears in adults, most frequently after age 40. A common name for it is “adult-onset” glaucoma.
Cause:
- PCG: Trabecular meshwork and Schlemm’s canal structural anomalies, which are present from birth, are the main causes of PCG. The anomalies cause the intraocular pressure to rise.
- POAG: Although its precise cause is unclear, POAG is frequently linked to age-related changes in the eyes. It frequently results in increased intraocular pressure due to reduced aqueous fluid drainage.
IOP, or intraocular pressure:
- PCG: PCG is characterized by an early-life onset, fast, and considerable increase in intraocular pressure.
- POAG: POAG often manifests as a slow-moving rise in intraocular pressure. It is frequently called “chronic” glaucoma.
Symptoms:
- PCG: In babies and young children, PCG symptoms may include excessive tears, photophobia (sensitivity to light), blepharospasm (closing of the eyelids), and an enlarged eye. Parents or other caregivers must watch out for these symptoms because infants cannot communicate them.
- POAG: In its early phases, POAG frequently exhibits no symptoms. Peripheral vision loss, trouble adjusting to low light, and, in more severe phases, tunnel vision, and central vision loss are possible symptoms of the disorder as it advances.
Diagnosis:
PCG: PCG is often identified when symptoms and clinical indications are seen in infancy or early childhood. Tonometry (the measurement of intraocular pressure) and gonioscopy (the examination of the drainage angle of the eye) are two examples of diagnostic procedures that may be used.
Adults who get routine eye exams frequently find out they have POAG before any symptoms become apparent. Measurements of intraocular pressure, examinations of the optic nerve, and testing of the visual field are all part of the diagnosis.
Treatment:
- PCG: Surgical surgery to establish a new drainage conduit for the aqueous humor is the main treatment for PCG. This can entail operations like trabeculotomies or goniotomies. Some patients could need ongoing care.
- POAG: Lowering intraocular pressure is the primary goal of treatment for POAG, which is frequently accomplished with the aid of eye drops, oral drugs, or laser therapy (such as trabeculoplasty). In more severe situations, surgery such as trabeculectomy or the insertion of drainage devices may be required.
Prognosis:
- PCG: Many people with PCG can preserve good vision and lead normal lives with early diagnosis and the right therapy. On the other hand, care and monitoring are frequently needed for life.
- POAG: To manage intraocular pressure and avert vision loss, POAG is a chronic condition that needs constant attention. Although the prognosis varies, prompt therapy can delay or stop the disease’s course.
PCG and POAG are different types of glaucoma with distinctions in beginning age, contributing factors, symptoms, diagnostic techniques, and therapeutic modalities. While POAG mainly affects adults and is frequently asymptomatic in its early stages, PCG mostly affects newborns and young children. To prevent visual loss, these disorders necessitate early diagnosis and adequate care.
Conclusion
Infants and early children are susceptible to the uncommon but deadly eye disorder known as primary congenital glaucoma. To maintain vision and avoid problems, prompt diagnosis and adequate treatment are crucial. While PCG can be difficult, improvements in medical and surgical treatments, together with the assistance of Low Vision programs, provide those who suffer from the condition hope. Those who have PCG can look forward to a brighter future with improved eyesight and a higher quality of life by staying informed and getting treatment as soon as necessary.
FAQs
Are there any treatments for primary congenital glaucoma?
PCG can be controlled but it cannot be cured. People with PCG can preserve good vision and enjoy normal lives with an early diagnosis and the right therapy.
Can changing one’s lifestyle help manage PCG?
A healthy lifestyle that includes frequent exercise and a well-balanced diet can support overall eye health, even if lifestyle changes alone cannot treat PCG.
Can PCG be found prior to birth?
If there are indications of eye enlargement or other abnormalities during prenatal ultrasound scans, PCG may occasionally be found. A conclusive prognosis, however, is typically made following childbirth.
Do those with PCG and limited vision have access to any support services?
Low eyesight services are one type of support service that can assist people with PCG to make the most of their remaining eyesight. These services could include counseling, therapy, and visual assistance.
Can PCG occur in adults?
Early childhood or infancy are the typical times for PCG diagnoses. The occurrence of PCG in adults is quite uncommon. Adults, however, are susceptible to different glaucoma types. For the detection and treatment of any eye disorders, routine eye exams are crucial.