Macular degeneration is a condition characterized by the deterioration of your central vision. This progressive eye disease can lead to loss of vision, which is why it’s so important to keep up-to-date with new treatments. Here are some of the most effective treatments for macular degeneration.
Ophthalmologists have been treating wet age-related macular degeneration (AMD) with monthly or bi-monthly eye injections for more than a decade, and dry AMD with antioxidant vitamins. When these medicines were originally launched, they offered hope for the first time that this sight-threatening condition may be delayed, halted, or even reversed. This movement is going through a fascinating transformation. So, what does the future hold for the 11 million Americans who suffer from AMD? We’ll get to it later, but first, some background information.
There are two types of AMD
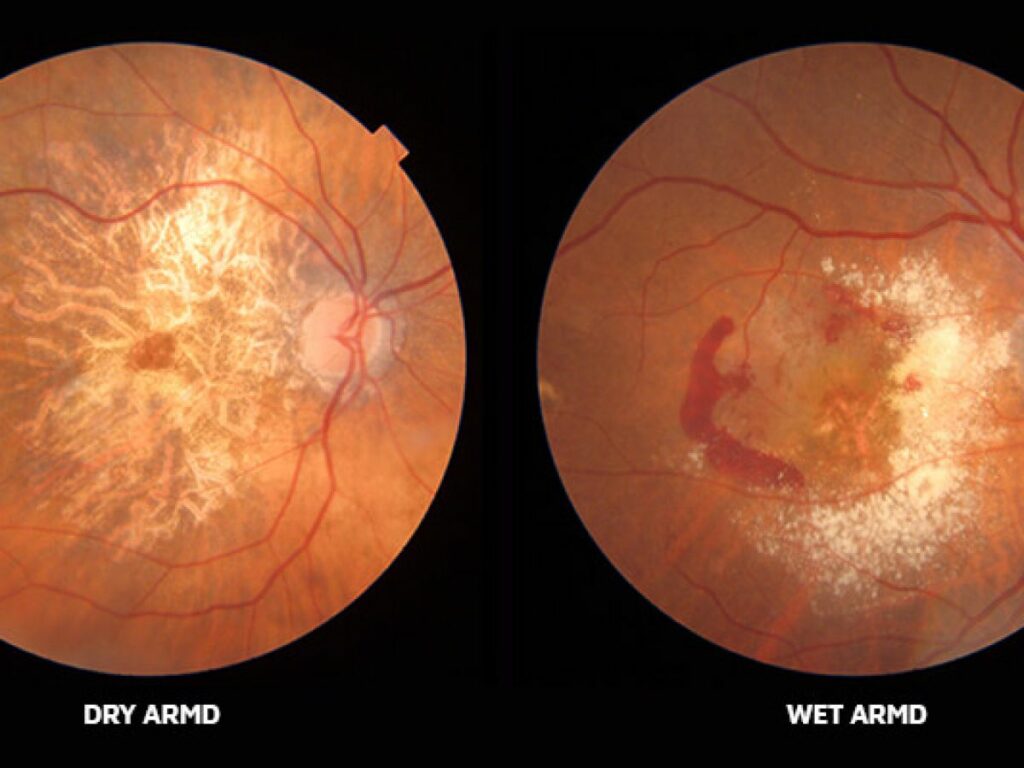
Wet Macular Degeneration
In the United States, wet age-related macular degeneration is one of the primary causes of low vision and visual loss.
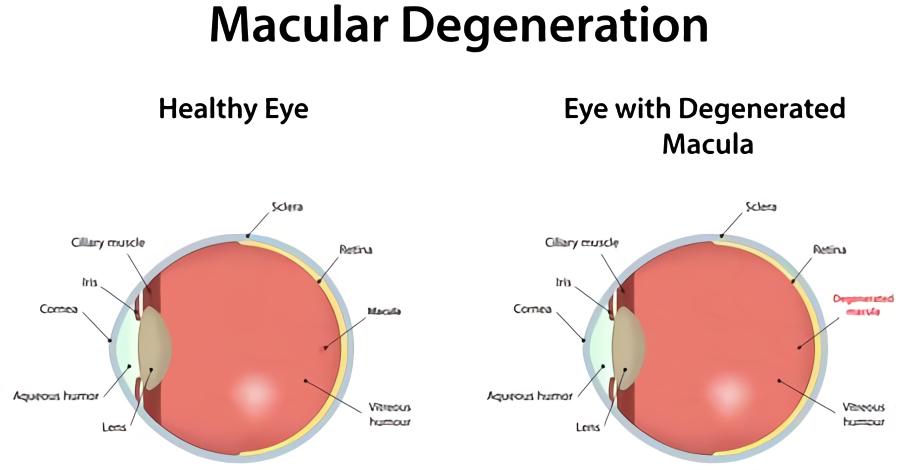
The formation of irregular blood vessels behind the retina causes bleeding, leakage, and scarring in wet AMD. People lose their center vision, which is required to discern fine details, as a result of this.
Scientists developed medications that interfere with this process by inhibiting a protein called vascular endothelial growth factor around 15 years ago (VEGF). People with wet AMD were most likely to experience significant vision loss or blindness before the development of these so-called anti-VEGF medications.
Then, in 2005, anti-VEGF medications made history by preserving the sight of wet AMD patients. In the overwhelming majority of patients, these medications help to stabilize or enhance eyesight. They must, however, be administered into the eye on a consistent basis.
The blood vessels in the retina’s walls might deteriorate and develop bulging pouches in diabetic macular edema. These may leak blood and other fluids, producing an enlargement of portions of the retina and visual impairment.
AMD and diabetic macular edema cause significant degeneration of central vision in the absence of effective control, resulting in difficulty reading, the potential loss of adequate vision for driving, and the inability to distinguish faces, but rarely to loss of peripheral vision, such that vision is generally adequate for safe self-care and walking unassisted.
Wet macular degeneration and (DME) diabetic macular edema are primary causes of blindness globally, affecting an increasing number of individuals. As a result, any breakthrough medications that can cure these illnesses are particularly welcome.
More long-lasting medications are now available, and treatments that may potentially cure the condition are under development. There is a lot of optimism for AMD patients.
While scientific studies suggest that anti-VEGF injections help more than 90% of patients preserve their eyesight, in the real world, the figure is closer to 50%. This is due to the fact that individuals are not getting treated as often as they should be. The issue is that most individuals need injections every four to eight weeks in order to maintain their eyesight. For many older patients who are suffering from various illnesses and need others to transport them to their ophthalmology appointments, this may be a tough schedule to maintain.
Dry Macular Degeneration
The center region of the retina, or macula, which is necessary for the clearest vision, is gradually damaged by age-related macular degeneration, which most usually affects those over the age of 55. Early AMD (also known as dry AMD) is the most common symptom. Dry macular degeneration is caused by a variety of factors that no one understands. However, research suggests that a mix of hereditary and environmental variables, such as smoking, obesity, and food, may influence it.
As the eye matures, the problem worsens. The macula — a region of the retina important for clear vision in your straight line of sight — is affected by dry macular degeneration. The tissue in your macula may atrophy or thin and lose vision-related cells over time.
AMD is a difficult condition with several causes. So far, we’ve learned that it’s caused by a lack (initially) of blood vessels, cell damage caused by free radicals (unstable molecules created by metabolic processes and environmental stresses), and the immune system attacking the retina.
Inflammation, lipids (blood fats), and maybe iron toxicity all play a role in AMD. Furthermore, persons with wet AMD have high amounts of C-reactive protein in their blood, which is a sign of inflammation. This shows that a broad inflammatory response is at play.
New Treatments for Wet Macular Degeneration
SusvimoTM (ranibizumab injection) 100 mg/mL was approved by the FDA on October 22, 2021, for intravitreal use via an ocular implant in people with wet or neovascular age-related macular degeneration (AMD) who had previously responded to at least two anti-vascular endothelial growth factor (VEGF) injections. In the United States, wet AMD affects roughly 1.1 million individuals and is the main cause of blindness in those aged 60 and over.
“Vabysmo is a significant stride forward in ophthalmology.” In a news release, Dr. Charles C. Wykoff, a Vabysmo phase 3 investigator and head of research at Retina Consultants of Texas, stated, “It is the first bispecific antibody licensed for the eye and a big development in treating retinal disorders such as wet AMD and diabetic macular edema.”
“With Vabysmo, we now have the chance to provide patients with a drug that may enhance their eyesight while also possibly reducing treatment burden by requiring fewer injections over time,” he said.
Similar drugs already exist, but they need more frequent injections into the eyes. Vabysmo treatment requires less frequent eye injections.
For those with wet AMD, the therapy consists of four monthly injections at first, followed by treatment every 2, 3, or 4 months, depending on the result.
A refillable medication reservoir is one intriguing option that might be accessible shortly. The anti-VEGF medicine Lucentis is stored in the port delivery system (PDS), which is a small refillable device. During a surgical operation, the port, which is about the size of a grain of rice, is inserted into the eye’s wall, just behind the eyelid. Over time, the gadget distributes medication into the back of the eye. Patients may have a fill-up once or twice a year at the doctor’s office instead of an injection every six to eight weeks. A specific needle may be used to replenish the device. According to the most recent research, many persons who were treated in this manner were able to go 15 months without treatments.
Anti-VEGF medications work because they focus on a single factor that causes wet AMD: VEGF. But what if a single medicine could address both of AMD’s basic causes? The medicine faricimab is based on this concept. Both VEGF and the protein angiopoietin-2 are targeted. It’s injected into the eye like any other anti-VEGF medication, but it lasts far longer. According to a new study, patients might wait up to four months between treatments. This information, however, is so recent that it has yet to be published in a peer-reviewed publication.
Beovu, a new medicine from Novartis, has been licensed for usage in the United States. About one out of every three Beovu patients can go up to three months without requiring another injection. In individuals with wet AMD, Beovu may perform a better job of drying retinal fluid than other medicines.
Abicipar, developed by Allergan, is still in phase 3 clinical studies and has yet to get FDA clearance. According to studies, this medicine permits patients to go three months without receiving an injection. This medication is also being studied for the treatment of macular edema.
Sunitinib, an injectable drug developed by Graybug Vision, has the potential to extend the time between treatments by 6 months. Sunitinab is now undergoing Phase 2B studies. It might take another 3 to 5 years before it becomes accessible.
The “complement cascade,” a component of the immune system, has long been suspected of being a factor in AMD. Two novel medications that target the complement cascade and prevent it from assaulting the retina are nearing the end of their clinical studies. One of the treatment candidates (pegcetacoplan, APL-2) targets the complement protein C3, while the other (Zimura, avacincaptad pegol) addresses a different protein in the cascade, C5. These medications are injected directly into the patient’s eye, much as the existing therapies for wet AMD. Researchers are currently looking at whether they may significantly increase eyesight in individuals after proving their safety. In roughly a year, the results should be available.
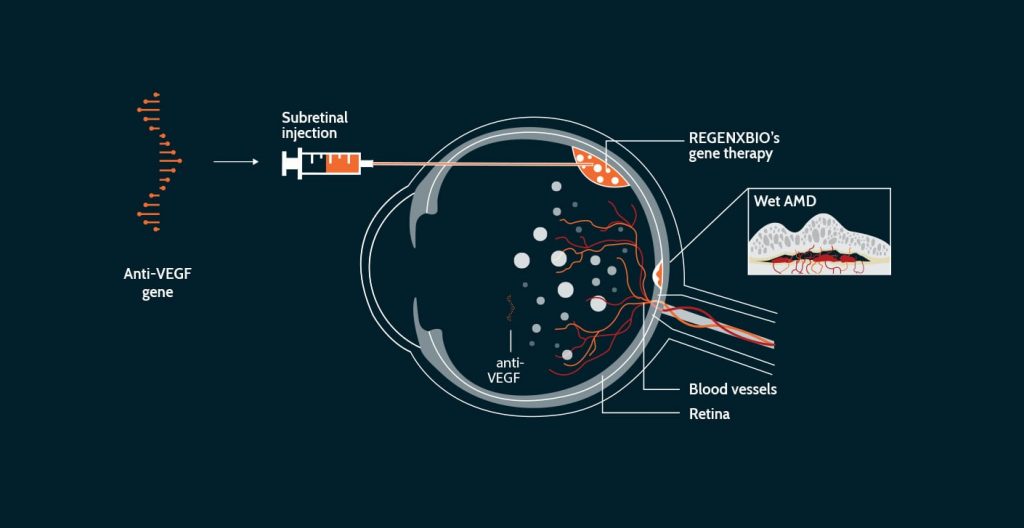
Gene Therapy for AMD
Gene therapy is a viable alternative to medications like Eyelea, Lucentis, and Avastin, which are injected into the eyes on a regular basis. Gene therapy aims to give a “one-and-done” treatment by assisting the eye in producing its own anti-VEGF medication. The gene therapy is being tested in two ways: one injects it under the retina in a surgical procedure, and the other injects it into the eye like a regular anti-VEGF treatment at the doctor’s office.
For wet AMD, there are four medication candidates under research, and one for dry AMD. Despite its potential, the long-term success of gene therapy needs to be established. One of the difficulties it confronts is the potentially exorbitant cost of such a therapy.
New Treatments for Dry Macular Degeneration
The dry type of AMD affects about 8 out of 10 patients with the disease. When sections of the macula atrophy (thin) with age, little clumps of a protein called drusen form. This is known as dry AMD. You gradually lose your core vision. Dry AMD is classified as early, moderate, or late-stage, according to its severity.
A mixture of antioxidant vitamins known as the AREDS2 formula may assist persons with the intermediate disease and lower their risk of vision loss. However, there is no therapy available for late-stage AMD, commonly known as geographic atrophy (GA). However, some promising clinical studies are now ongoing.
Another idea being looked at involves replacing some of the cells that start to die in late-stage dry AMD. Stem cells may be able to restore the retinal cells that have died as a result of the illness. These stem cells are being transplanted into the eye by doctors. Layering stem cells on thin scaffolds is one technique. Another option is to dissolve the cells in a fluid solution and inject it under the retina. Small clinical studies have shown that stem cells do not have any unanticipated negative effects. These therapies may take ten to fifteen years to fine-tune and prove successful in people.
Nutritional and vitamin therapy To delay dry AMD, several improved fish oils and AREDS 1 and 2 vitamins — compounded with zinc, lutein, zeaxanthin, and other compounds — are now commonly used as tablets. Despite its effectiveness, a research study published in December 2020 in the journal Oxidative Medicine and Cellular Longevity advised that the supplement didn’t completely prevent intermediate AMD development over an eight-year timeframe. Given the established correlations between wet AMD, a Western-style diet, and other systemic illnesses, Dunaief believes that other dietary connections may provide further nutritional therapy options. Researchers discovered that adhering to a diet rich in healthy nutrient-rich foods such as fruits, vegetables, legumes, and seafood lowered the chance of progression to advanced AMD by 41% among the more than 4,000 participants in a 2018 study published in Ophthalmology (all over 55).
New low vision technology
For those whose disease has progressed to the stage that can no longer be treated by any of the current or new medical treatments for macular degeneration, there are exciting new devices and software programs to help keep you active, independent and doing the things you love. Vision buddy is a device that plugs into your tv streaming device and allows you to watch TV in the headset. It also has a portable stand with a camera to replace CCTVs and a way to plug into your computer to magnify and view it through the headset also. Another cool product is the EZReader system which makes using a computer much easier and more visible with large icons, apps, and high contrast colors.
FAQ’s
How close is a cure for macular degeneration?
Although gene therapy has exciting potential, it is still very early in the studies to say if it will be a “cure”. It is very expensive and the trials have many years to go to be conclusive.
Does AMD make you go completely blind?
Both forms of AMD causes central vision loss which is very damaging to your functionality. It may impair your ability to make out faces, read, or drive. As serious as that is, the disease isn’t a lights-out disease that makes you go completely blind. Assuming you don’t have other ocular conditions like glaucoma or cataracts your peripheral vision will remain intact.
Can macular degeneration be cured with stem cells?
As mentioned above, there is exciting progress being made with stem cells. These new treatments for macular degeneration are still new and being studied. Time will tell.
Which is worse: dry or wet macular degeneration?
Generally speaking, the wet form tends to be the worst and most progressive form of AMD. However, for some the end stage of dry AMD where the retina thins and a large area of retinal atrophy takes place, the vision can end up just as bad as in the end-stage of the wet form.
Can laser treatment help macular degeneration?
Laser treatment is another effective treatment to help slow the progression of AMD. It, unfortunately, isn’t a cure though. The laser can slow the progression of the blood vessel growth but it does thermal damage to the retina in the process and leaves blind spots where it is applied.