A series of genetic eye conditions known as juvenile macular degeneration (JMD), sometimes known as juvenile macular dystrophy, can affect children and teenagers.
The macula, a portion of the retina, is damaged by all kinds of JMD, despite the fact that they all behave differently. Our center vision is controlled by the macula, which also enables us to perceive fine details.
Right now, JMD is incurable. Even while some people have had steady eyesight for years, it can eventually lead to irreversible visual loss. Early diagnosis might aid youngsters in adjusting to and managing visual loss.
We’ll discuss the primary JMD varieties’ symptoms, their underlying causes, and available management choices.
Juvenile macular degeneration: what is it?
The eye’s macula deteriorates as a result of this condition. The area of the retina known as the macula is responsible for center vision and gives us the ability to clearly discern minute details.
When the macula—the portion of the retina that allows for lateral vision—is damaged, the quality of vision suffers because it is much more used for detail than the rest of the retina.
When the macula is damaged, the center vision is compromised, which results in blurry and unfocused vision.
The three primary categories of JMD are:
- Stargardt’s disease
- X-linked Retinoschisis
- Best’s disease also known as vitelliform macular dystrophy
While the central vision is altered by all types of juvenile macular degeneration, the symptoms and course of the disease differ greatly. Some kids won’t discover changes in their eyesight until an eye exam, while other youngsters will sense a deterioration in their vision. The rate of eyesight loss differs as well.
Stargardt Disease Symptoms
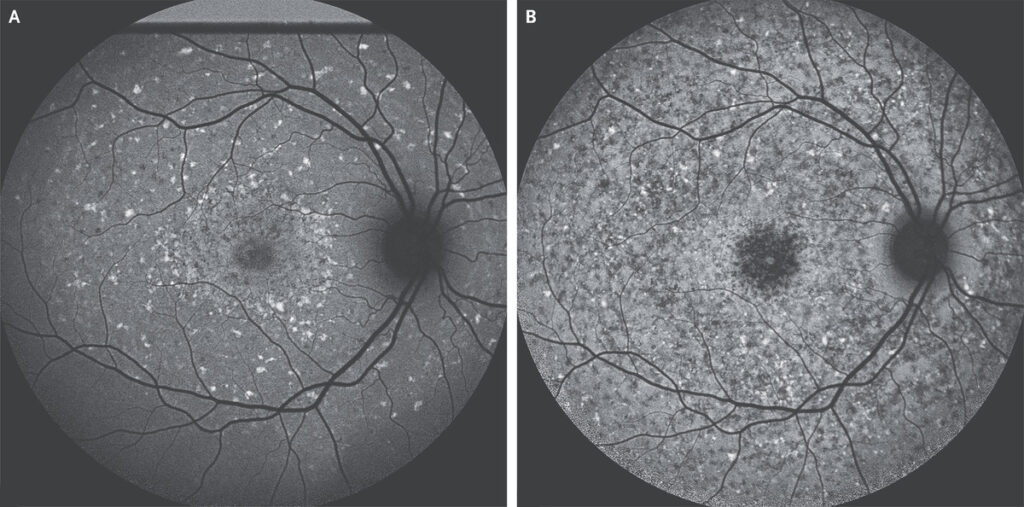
Stargardt disease, commonly referred to as fundus flavimaculatus, is one variation of JMD. Though vision loss may not be apparent until the 30s, the condition typically begins before the age of 20. Many individuals retain their peripheral vision but experience central vision loss to the 20/200 range. A dilated ophthalmoscope eye exam can reveal the disease’s distinctive pattern of white “flecks” in the retina, which eye professionals can use to make the diagnosis.
Genetics of Stargardt Disease
The ABCR gene’s recessive mutations are often the source of the illness. One-quarter of the offspring of parents with one mutant copy of the ABCR gene will develop the condition. Unless the spouse also possesses the recessive ABCR gene mutation, a child with Stargardt disease who carries two copies of the mutation is unlikely to have afflicted children (which is rare). People who have ABCR gene mutations build up A2E, a dangerous toxin, in their retinas. ABCR often prevents A2E from forming. Utilizing sunglasses to block out light may lower the development and toxicity of A2E.
Best’s disease symptoms
- Best vitelliform macular dystrophy (BVMD). This is used to describe diseases brought on by modifications to the BEST1 gene.
- Between the ages of 3 and 15, the macula starts changing with this disease, and it may impact 1 to 9 out of every 100,000 persons.
- For decades, a person with Best’s disease may have normal eyesight and not detect any vision loss. Many sufferers aren’t aware of their problem until a doctor doing an eye check finds it.
- Under the macula, the patient may have a yellow cyst that resembles a sunny-side-up egg. This cyst contains lipofuscin, a fatty yellow pigment. When a cyst bursts, it will leave behind yellow deposits that resemble scrambled eggs.
Other BVMD signs and symptoms include:
fuzzy vision
One eye, or in bilateral situations, one eye more severely than the other, loses central vision but not peripheral vision.
Juvenile X-linked retinoschisis symptoms
Research from 2012 indicates:
- This disease often affects people who are male since it is associated with a mutation in the X chromosome.
- Before kids are old enough to start school, X-linked juvenile retinoschisis (XLRS) is frequently diagnosed, and it has even been found in neonates.
- According to the National Organization for Rare Disorders, kids may struggle to read aloud in class or see the blackboard, and glasses do not help.
Additionally, some kids with XLRS may show:
- nystagmus (a type of scanning or involuntary movement of the eyes in a rapid back and forth motion)
- farsightedness (difficulty seeing up close)
- Eyes crossing or not aligned in the same direction which is referred to as strabismus
- Variable vision loss is caused by XLRS. While some people maintain their eyesight for their whole lives, others lose their vision quickly during the first decade or two.
Causes of Juvenile Macular Degeneration
All kinds of juvenile macular degeneration are brought on by mutations in one or more genes.
Causes of Stargardt’s disease
According to the National Eye Institute, mutations to the ABCA4 gene, which alters how your body utilizes vitamin A, cause Stargardt disease.
ABCA4 is meant to produce a protein to remove fatty materials (lipofuscin) that accumulate on the macula. The gene cannot carry out this function as a result of mutation.
Lipofuscins accumulate and ultimately damage light-sensitive cells known as retinal pigment epithelium (RPE). Loss of center vision results from this.
Causes of X-linked retinoschisis
X-linked retinoschisis (XJR) is caused by mutations in the RS1 gene, which is found on the X chromosome. Retinoschisin is a protein that is produced by the RS1 gene and is thought to aid in retinal maintenance.
Only patients with XY chromosomes, which are seen in males, exhibit this kind of JMD. XX chromosome carriers, who are female, can carry this mutation but typically don’t show any symptoms.
There may occasionally be an X-linked retinoschisis instance without an RS1 mutation. It is unclear to experts what causes these occurrences.
Causes of Best vitelliform macular dystrophy
A change in the VMD2 or bestrophin gene is what causes best vitelliform macular dystrophy (BEST1).
Since only one copy of the defective gene is required to produce the ailment, it is known as an autosomal dominant genetic disorder. Regardless of sex, anybody can be impacted.
One in 10,000 people will get Best’s disease, and the onset usually happens between age five and ten.
Diagnosis of Juvenile Macular Degeneration
To examine the retina, your ophthalmologist will do a dilated eye exam. Juvenile macular dystrophy patients exhibit symptoms unique to their condition.
Yellowish specks in and under the macula are possible in those who have Stargardt disease. These specks can occasionally radiate in a ring-like pattern. Lipofuscin, a fatty consequence of typical cell activity, is what the flecks are made of. Patients with Stargardt disease experience excessive lipofuscin buildup.
Under the macula, a yellow cyst develops in Best’s disease sufferers. When the cyst ultimately bursts, fluid, and yellow deposits are released. These could cause macula damage.
The macula is impacted by the retina splitting into two layers in juvenile retinoschisis. Blisters may develop in the gaps between these layers. The vitreous, the liquid that fills the eye, is susceptible to blood vessel leakage. Retinal detachments may result from juvenile retinoschisis.
To confirm the diagnosis, your ophthalmologist or optometrist could do an OCT or fluorescein angiography, a laser scan of the retina. A dye is injected into your arm during this examination. As the dye moves through the blood vessels in your retina, a picture of it is taken. ERG (electroretinography) testing may also be recommended by your doctor. The retina’s electrical activity is assessed during this examination. Genetic testing is currently done in specialized labs. They are able to identify the precise gene responsible for the illness. Knowing this is crucial since various genes might result in the same retinal appearance.
What is the treatment for juvenile macular dystrophy?
Juvenile macular degeneration is still incurable. But several clinical studies for gene therapy are now being conducted. It is possible to treat the faulty gene in the retina with gene therapy. These therapies might be able to halt the disease’s development and stop visual loss.
Genetic Counseling for JMD
To determine whether additional family members are at risk for certain diseases, genetic counseling is highly beneficial.
Treatment of Wet AMD developing from Juvenile macular degeneration
Sometimes patients with Best’s illness or Stargardt disease will see the formation of new blood vessels (neovascularization) in the macula. Like wet AMD, these vessels have the potential to bleed and leak. Similar to AMD, injection of medications that inhibit vascular endothelial growth factor is the therapy for new blood vessel formation and leaking in the retina (VEGF). These medications include ranibizumab (Lucentis®), aflibercept (Eylea®), pegaptanib sodium (Macugen®), and brolucizumab (Beovu®).
Low Vision Aids
Low vision assistive devices can help patients who have lost their central vision. An optometrist specializing in low vision can prescribe these. They consist of both electronic magnifiers that can magnify items and specialized magnifying glasses that may be worn or handled.
Telescope glasses called Bioptics are a great option for students to be able to see the board in school, drive a car, or even spot faces from across the room faster. Assistive applications for their phones and computers can enlarge the print, read the words
The mental health of a JMD Patient
Experiencing vision change or loss can be stressful and upsetting for anyone.
Children and teens will need emotional support from family and friends while they manage JMD. You may also consider consulting a therapist to help them with coping techniques, stress relief, and more.
Anyone who experiences a change in or loss of eyesight may feel anxious and worried.
While managing JMD, children and teenagers will require emotional support from family and friends. You may also think about having a therapist aid them with coping mechanisms, stress management, and other things.
AMD and JMD
Age-related macular degeneration (AMD), a prevalent eye disorder that affects people as they age, is distinct from JMD.
A gene mutation is the only known cause of hereditary juvenile macular degeneration. Age-related macular degeneration, in contrast, occasionally lacks a hereditary component. AMD is often brought on by the macula’s natural deterioration brought on by age.
Conclusion
Monitoring a child’s visual development is crucial. This is especially true if they have a family history of eye disorders. If your kid complains of haziness, spots, or any other changes in vision, take them for routine eye exams and have them checked.
By safeguarding their eyes, and employing adaptive technology, and low vision aids, you can help your kid with JMD have the best possible vision. To provide your kid or teen further emotional and psychological assistance while they cope, think about seeing a therapist.
Although there is no known treatment for juvenile macular degeneration, the rate and degree of visual loss might vary greatly. Some persons with JMD have steady eyesight for years or decades; not everyone with JMD loses all of their vision.
FAQ’s
Can macular degeneration happen in teens?
Yes, Both Stargardt Disease and Best’s Disease can occur in teens. Juvenile Retinoschisis usually occurs earlier.
Can early-stage Juvenile Macular Degeneration be reversed?
No, unfortunately, However gene therapy treatments are showing promising results to minimize the damage from the diseases associated with it.
Do you always go blind with macular degeneration?
No, The severity of each disease can be quite different for each person. None of the 3 primary causes of Juvenile Macular Degeneration cause complete blindness. But can potentially cause legal blindness due to the central vision being reduced to 20/200 or worse. But it doesn’t cause complete blindness with no light perception of peripheral vision.
Can Juvenile macular degeneration be cured?
Not at this time. Gene therapy is showing promise though.
At what age does macular degeneration usually begin?
Each of the different conditions has different time frames for symptoms to start. Read above for the age ranges for each.