Glaucoma is a condition that involves the loss of optic nerve function and vision loss. It can be treated but if it is left untreated, it will lead to permanent and irreversible blindness. This disease can be detected by a series of tests which includes visual field testing, and optic nerve head cupping test. These are tests that are done by doctors or low vision specialists. This blog gives you detailed information about “how to test for glaucoma”.
What exactly is glaucoma?
Glaucoma is a catch-all name for a collection of disorders that have a common pattern of optic nerve damage. The optic nerve is a bundle of nerve fibers located in the back of the eye that transmits visual information from the retina to the brain. Clinical examinations can classify several different kinds of glaucoma. Primary open-angle glaucoma is the most prevalent kind (POAG). POAG patients often have no symptoms at all until the illness has progressed to an advanced stage. Side vision loss and poor visual quality are the most typical signs of advanced illness, which may considerably affect everyday activities, including driving. Current therapies have shown to be beneficial in delaying the progression of the illness, but not in restoring optic nerve damage.
Glaucoma comes in a variety of forms
The most prevalent kind of glaucoma is primary open-angle glaucoma. Because fluid cannot drain correctly, the pressure inside increases, placing strain on the optic nerve.
Acute glaucoma, also known as angle-closure glaucoma, is a less prevalent kind of glaucoma. The area between the iris and the lens abruptly closes, causing the anterior chamber to fill with fluid, even when the drainage ducts are functioning properly.
When the angle narrows, the aqueous fluid gets obstructed, placing pressure on the optic nerve, kind of like standing on a hose. Acute angle-closure glaucoma is a very serious medical emergency that must be treated right away. Symptoms that are common include Nausea, Eye pain, redness, blurred vision, and headaches.
Normal-tension glaucoma does not raise eye pressure, yet it still damages the optic nerve. The drainage ducts are in good working order, and the distance between the iris and the lens is adequate, but the optic nerve is still compromised. Normal-tension glaucoma is more common in certain persons than in others.
What are glaucoma tests and how do they work?
The key to preserving your eyesight against glaucoma damage is early identification, which may be achieved via frequent and comprehensive eye examinations. Five typical glaucoma tests are included in a glaucoma workup.
Exam with dilated pupils.
Prior to your first consultation, get your medical documents from your previous and/or current eye physicians and ensure that they have been received (or better yet, bring the records with you). Previous eye pressures, maximal eye pressures, past surgery or laser operations, and prior testing (visual field, disc pictures, or optical coherence tomography) should all be included in these records (OCT).
Glaucoma tests are a collection of tests used to identify glaucoma, an eye illness that may result in vision loss and blindness. Glaucoma develops when fluid accumulates in the front of the eye. Eye pressure rises as a result of the excess fluid. The optic nerve may be damaged by increased eye pressure. The optic nerve is responsible for transmitting information from the eye to the brain. Damage to the optic nerve may result in major visual issues.
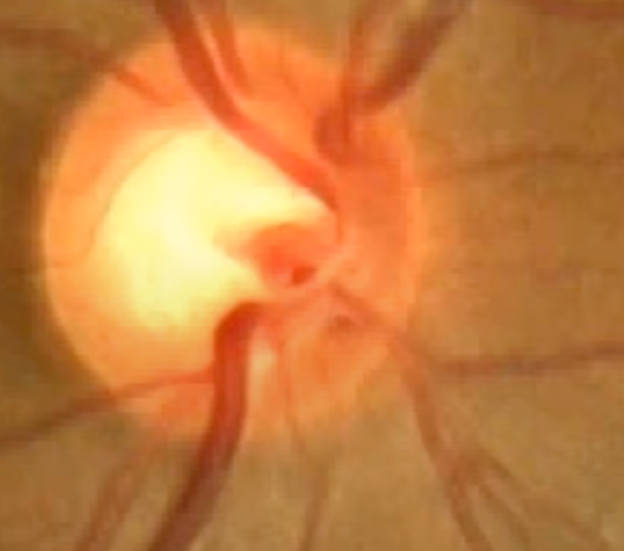
An ophthalmoscope is a piece of simple equipment that may be used to examine the optic nerve in a clinic setting. The optic nerve leaves the eye in the back. The nerve is made up of about one million distinct nerve fibers that begin in the retina (the light-sensitive layer covering the interior of the eye) and go to different parts of the brain. The optic nerve may be seen (optic nerve head) and the nerve fibers can be seen weakly fanning out onto the retina while looking into the eye.
This diagnostic process allows your doctor to check for glaucoma damage in your optic nerve. Eye drops dilate the pupil, allowing the doctor to check the structure and color of the optic nerve in your eye.
Your vision may be blurry and you may be more sensitive to light while your eyes are dilated. These side effects may linger for many hours and are of varying degrees of severity. Bring sunglasses to wear after the appointment to protect your eyes from harsh light. You should also plan for someone to take you home since your eyesight may be too blurry to drive safely.
Six Glaucoma Tests
Comprehensive eye exam
As previously stated, a full eye exam is required.
Tonometry
This glaucoma test checks the intraocular pressure in your eyes.
Glaucoma is caused by an increase in ocular pressure, which is the major risk factor. When you see your eye doctor, it is considered one of the “vital symptoms.” Just as high blood pressure is a risk factor for stroke, high eye pressure is a risk factor for glaucoma. The most frequent way of measuring ocular pressure is “applanation,” in which a small tool meets the surface of the eye after it has been numbed with an eye drop. It’s painless and fast, but it does need your participation. Knowing this is useful since the reading might be inaccurate if you are not completely calm at the moment of measurement. It’s also crucial to keep breathing during the assessment.
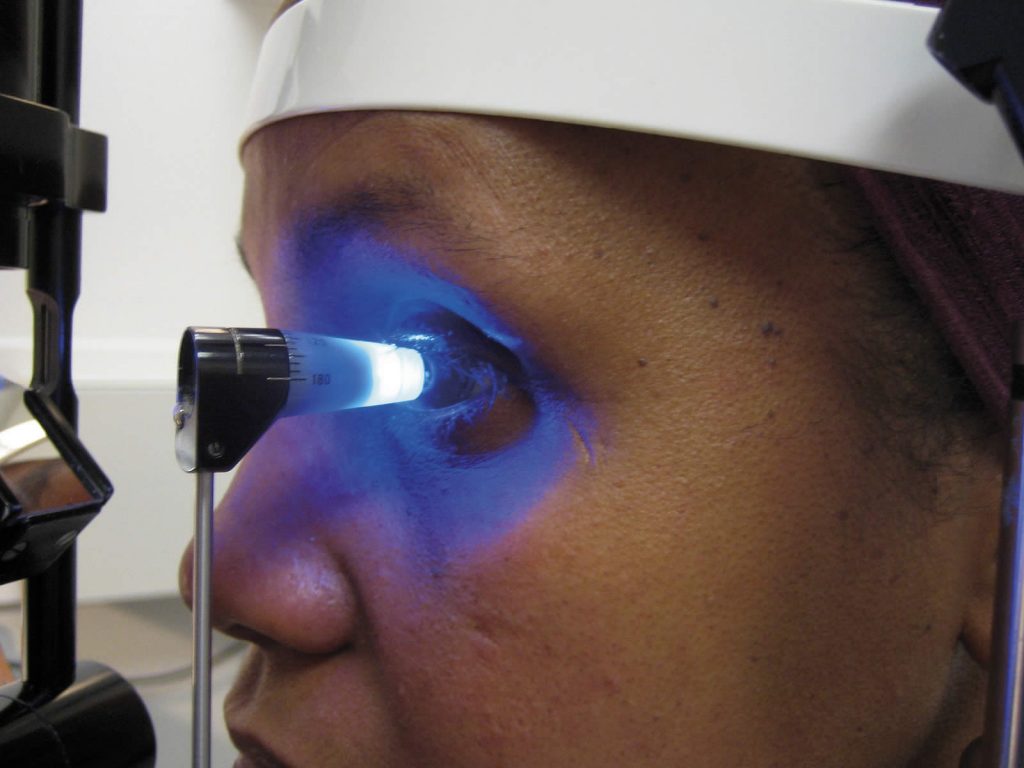
The Goldmann applanation tonometer is the most widely used method for determining IOP. A little sensor on an arm pushes on your tear film, measuring a pressure under blue light using a microscope.
A typical kind of pressure testing is done with the NCT (non-contact tonometer).
To test your internal eye pressure, a blast of air flattens the cornea. Non-contact tonometers don’t generally need numbing eye drops. They’re used in a lot of clinics for screening.
Normal-pressure ranges from 12 to 22 mm Hg (“mm Hg” refers to millimeters of mercury, a scale used to measure ocular pressure). When the pressure in the eye exceeds 20mm Hg, glaucoma is suspected. Some individuals, however, might develop glaucoma at pressures ranging from 12 to 22 mm Hg. Each person’s eye pressure is different.
Gonioscopy
Another test conducted by your doctor using a hand-held gonio lens is gonioscopy. The lens is also known as an “exam contact lens” by certain clinicians. The gonioscopy lens will slightly touch the numbed cornea by the doctor. The operation is straightforward, fast, and painless. It’s comparable to how a periscope uses mirrors to observe locations that aren’t visible to the human eye. When the gonioscopy lens comes into contact with the cornea, the eye doctor will be able to observe the “angle.” The “angle” is the point where the cornea (the transparent front section of the eye) meets the iris (the colored component of the eye) (the colored part of the eye). The trabecular meshwork (drainage structure of the eye) is likewise situated at the “angle.” Under normal conditions, the bulk of the fluid produced within the eye must travel through the trabecular meshwork to leave the eye. On gonioscopic inspection, if the trabecular meshwork is visible, clinicians refer to this as an “open” angle. A “closed” angle occurs when the trabecular meshwork is occluded by scar tissue or the iris.
You’re more likely to have a quick or abrupt spike in your IOP if the angle is closed and blocked. In addition to examining the angle, gonioscopy may detect any irregular blood vessels or trauma-related damage.
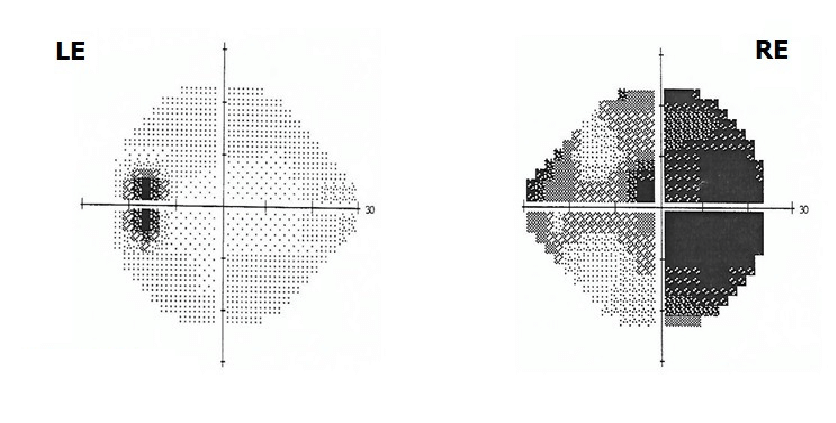
Visual Field Testing
Perimetry is a visual field test that generates a map of your whole visual field. This test will assist a doctor in determining whether or not you have glaucoma. You will be asked to stare straight ahead as a light spot is repeatedly displayed in various locations of your peripheral vision throughout this test. This aids in the creation of a “map” of your vision.
If you notice a delay in seeing the light as it passes into or around your blind area, don’t be afraid. This is completely normal and does not indicate that your range of vision has been harmed. During the exam, try to relax and react as precisely as possible.
Your doctor may request that you repeat the test to determine whether the findings are the same the second time around. Visual field tests are normally done once or twice a year after glaucoma has been diagnosed to check for any abnormalities in your eyesight.
The visual field test is a functional exam that enables your doctor to evaluate whether you have lost any field of vision due to glaucoma, how much you have lost, and the pace of disease development, all of which can assist and help customize your therapy. Based on the results of this test, your doctor will be able to determine the severity of your condition.
Although the test is painless and takes just a few minutes for each eye, if you are worried or sleepy, you may not be able to complete it accurately. In addition, the exam may have a learning curve and so may need to be repeated. There is no need to remove your contact lenses or prepare for the exam in any way. The visual field test should be conducted on a regular basis, albeit the frequency may vary based on your unique condition.
Corneal Thickness Examinations
Pachymetry is a painless test that determines the thickness of your cornea, which is the transparent window in front of your eye. To measure the thickness of the cornea, a probe called a pachymeter is gently placed on the front of the eye. Because corneal thickness has the ability to alter ocular pressure measurements, pachymetry may aid in diagnosis. Your doctor can better assess your IOP measurement and establish a treatment plan that is suited for you using this measurement. The method to measure both eyes takes around a minute.
Corneal thickness may make it difficult to get a precise measurement of your IOP, resulting in a misreading of the internal pressure. There is a risk of misdiagnosis if your eye doctor does not consider your corneal thickness. You may get an accurate diagnosis by measuring the thickness of your cornea and taking an exact ocular pressure reading.
Pachymetry is also used in analyzing your risk assessment if you are borderline on some of the other tests. There is a strong clinical association between thick corneas and thick sheeting of the nerve fibers which protect the nerves. So the thicker the cornea, the less likely there is going to be nerve damage from increased pressure.
Imaging Tests for Glaucoma
Fundus photos are used to track a patient who is suspected of having glaucoma or who has been diagnosed with glaucoma. Doctors may compare future pictures to images taken previously by capturing the optic nerve at a specific moment in time. This comparison is very useful in detecting optic nerve progression and selecting between medication and surgical glaucoma treatment options.
Glaucoma imaging exams are a reliable technique for your doctor to track the development of glaucoma. The tests are non-invasive and do not expose you to any radiation. Your pupils will be dilated with eye drops, and the doctor will image your optic nerve (ON) with a digital camera or map your optic nerve using other technologies (OCT). The data are instantly accessible, regardless of the modality your doctor selects, and may be presented on a computer screen for review.
Nerve Fiber Analysis
Nerve fiber analysis is a recent glaucoma diagnostic procedure that measures the thickness of the nerve fiber layer.
Thinner regions might suggest glaucoma-related damage. This test is particularly useful for people who may be suspected of having glaucoma, as well as for determining if a person’s glaucoma is worsening.
Over one million distinct nerve fibers/axons make up the optic nerve. Because nerve axons cannot be precisely measured in a live eye, indirect axon measurements (axon “counting”) must be performed. Clinical practice presently employs optical coherence tomography (OCT), GDx Analyzer (short for Glaucoma Diagnosis Analyzer), and Heidelberg Retinal Tomography (HRT). Currently, the most common method utilized by glaucoma experts for optic nerve fiber examination is optical coherence tomography (OCT).
Results of glaucoma testing
Combining the information from all of the glaucoma tests helps to determine if one has glaucoma. Since glaucoma is a very slow progressing disease it can be difficult to accurately determine in the early stages if the damage is occurring. With careful monitoring of the results of these tests over time, your doctor or low vision specialists can accurately determine if the damage is occurring to your nerves in the back of your eyes. This is why regular eye exams are so important. If you are a glaucoma suspect or have a family history of glaucoma. You should be diligent about having your eyes checked every year. If you aren’t in either of these categories you should at least have your eyes checked every two years up to the age of 50 and every year after that.
FAQs about Glaucoma testing
How to test for glaucoma at home?
There really aren’t at-home glaucoma tests, unfortunately. If you notice that your eyes throb a lot or your peripheral vision isn’t great then you should see your doctor.
How much does it cost to get tested for glaucoma?
To have all the testing done required to get an accurate diagnosis for glaucoma. It will cost between $300-500 dollars.
How can I test myself for glaucoma?
As mentioned above there is no way to test yourself aside from being aware of the symptoms.
What is the most accurate test for glaucoma?
Of all the tests done for glaucoma, the OCT gives the most accurate data for diagnosing glaucoma.
How many years does it take to go blind from glaucoma?
Every patient and their disease progression is different. Much of it depends on how early it is detected and treatment is started. Glaucoma is generally a very slow progressing disease but left untreated can cause considerable damage in just a few years.