Anatomical narrow angle glaucoma is an eye condition that is not as well known, yet very significant. This greatly misunderstood eye condition deserves attention and comprehension. In this article, I will be exploring the various facets of anatomical narrow angle glaucoma-from its definition, to treatment, to lifestyle management-to equip you with all the information necessary for you to be an expert!
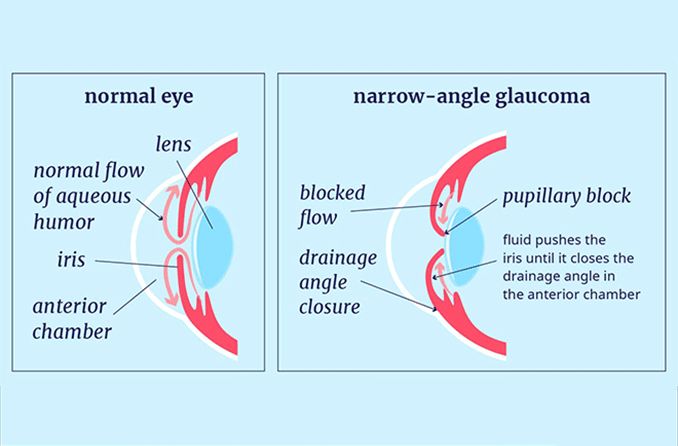
An anatomically narrow angle could be described as an anatomically abnormal eye condition with impaired drainage and this one is later classified into two types: angle closure and angle closure glaucoma. The drainage angle is a section inside your eye where the cornea and iris meet.
An understanding of the anatomy of the eye is needed to comprehend anatomical narrow angle glaucoma. The drainage angle, which is between the cornea and iris, needs to remain open and unaffected in order to prevent total blockage of intraocular pressure. In this condition, the drainage angle is narrower than normal which obstructs the outflow of the fluid, causing a slow increase in pressure inside the eye.
Causes and Risk Factors for Anatomical Narrow Angle Glaucoma
While anyone can be stricken by glaucoma, there are a few factors to determine if someone is more likely to be starting anatomical narrow angle glaucoma. These factors will not be able to 100 percent determine if you will be getting glaucoma but it can help determine if you are at higher risk. Some of these factors can include the following.
Age
As age increases the portion of Persons at risk of glaucoma will rise. As we age our eye anatomy changes, resulting in an increased risk of glaucoma in a few adults. A common alteration in the eye anatomy that raises the risk of glaucoma is the narrowing of the eye’s drainage angle.
With this disease, you may have the factors of genes that had this problem with glaucoma. “Anatomically narrow angle glaucoma or primary angle-closure glaucoma is more common in individuals with a family history of this type of glaucoma.” Primary angle-closure glaucoma is much more common in families showing the genetic background of these family members.
If you are hyperopic, or farsighted, you may have a higher risk of developing anatomically narrow angles. The shape of the eye that is common in patients that are hyperopic may cause a crowding of the outflow of the eye.
A possible racial or ethnic factor is a matter of debate, but some studies have suggested that individuals of East Asian descent may have a higher proportion of narrow angles, while those of African descent may have a higher mean IOP.
Gender
Studies have shown conflicting results as to whether it is men or women who are at the highest risk for developing the anatomical narrow angle glaucoma disorder. However, women may be slightly more at risk due to hormonal changes, especially during the changes occurring during menopause.
There are certain anatomical variations (in the structure of the eye) that may also lead to a more narrow angle. These variations can be present from birth or may develop later in life and put a patient at a greater risk for developing angle-closure glaucoma.
Location
The prevalence of narrow angle glaucoma may vary depending on the location within the world. There could be a link between the latitude or weather conditions and why they develop this condition.
It is important to note that these factors do not increase the risk for anatomical narrow angle glaucoma 100% and a person who does not have these risk factors may still develop the condition. It becomes increasingly important to receive regular eye examinations with age to increase the chances of a prompt diagnosis and treatment.
When a family history of glaucoma or an individual has one or more risk factors, then we need even more attention on routine eye check-ups. Early detection and treatment would prevent the progression of anatomical narrow angle glaucoma and complications.
Symptoms and Diagnosis
Some people with anatomically narrow angles may not have symptoms unless the angle between the iris and cornea closes. Symptoms include severe eye pain, headache, blurred vision, rainbow-colored halos around lights, and nausea and vomiting. Immediate, correct diagnosis is important because treatment with medications and sometimes surgery can help prevent damage to the optic nerve. Your eye health care provider will take a complete medical history and do a thorough eye exam, including measuring intraocular pressure, evaluating the drainage angle, and assessing the appearance of the optic nerve.
Treatment Anatomical Narrow Angle Glaucoma
Treatment considerations for anatomical narrow endpoint glaucoma are based on a step-wise approach. The first step to managing this condition is the reduction of intraocular pressure. There are several management options for anatomical glaucoma narrow endpoint some include medications to lower the intraocular pressure, bicarbonate, laser therapy also known as laser peripheral iridotomy creating a hole in the peripheral iris, and in some cases surgical interventions to enhance drainage. Management options for anatomical narrow endpoint glaucoma depend on your management of the conditions and are tailored to the patient’s condition
Complications and prognosis
Complications may develop if anatomical narrow angle glaucoma is not diagnosed and managed in a timely manner. Failure to address anatomical narrow angle glaucoma can lead to serious complications, such as permanent loss of vision. Optic nerve damage resulting from long-term high intraocular pressure can lead to permanent visual impairment if it persists. However, if treated promptly and appropriately, the prognosis is good in the case of anatomical narrow angle glaucoma. This underscores the importance of early identification and treatment.
Aside from medical and surgical management, patients with anatomic narrow angle glaucoma can also manage the disease by virtue of their lifestyle. To warrant good eye health and well-being, patients should undergo regular eye check-ups and should fully comply with all prescribed medications. Maintaining good health can be achieved by living a healthy lifestyle. Regular exercise and a balanced diet are advisable. Patients must be aware of the specific position that they choose, as there are certain positions in doing yoga that result in a significant increase in intraocular pressure and might compromise patients with anatomic narrow angle glaucoma.
Anatomical Narrow Angle Glaucoma vs Primary Open Angle Glaucoma
Having a clear understanding between anatomical narrow angle glaucoma and primary open angle glaucoma (POAG) is very important for proper diagnosis and treatment. While both of these fall under the same classification of glaucoma they do have some distinct differences in relation to the anatomy of the eye and the mechanisms that cause the intraocular pressure to go up.
Anatomical Narrow Angle Glaucoma
This type of glaucoma is characterized by a narrow drainage angle between the iris and cornea which blocks normal fluid outflow and increases intraocular pressure.
Primary open-angle glaucoma (POAG)
In primary open-angle glaucoma (POAG), the drainage angle formed by the cornea and iris remains open, yet the trabecular meshwork is partially blocked. This causes pressure in your eye to gradually increase, which can damage the optic nerve.
Anatomical Glaucoma, Closed-Angle Glaucoma, Acute Glaucoma This type of glaucoma is often presented with acute symptoms and is considered a medical emergency particularly when there is a sudden blockage of the drainage angle which is called acute attack glaucoma. Acute attack glaucoma is the name applied when symptoms build up very rapidly, produce severe pain, and damage the eye. These symptoms could include severe pain in or around the eye, headache, visual disturbance such as blurred vision or seeing rainbow-like halos around lights, and in more severe cases nausea.
Typically POAG progresses slowly and in most cases is asymptomatic in its early stages, therefore most individuals with POAG don’t notice any change in vision until optic nerve damage has developed enough to affect their peripheral vision.
Anatomical Narrow Angle Glaucoma: The condition is more common in older patients, Age is a significant risk factor. Other risk factors include hyperopia (farsightedness), a family history of Narrow angle glaucoma, and certain anatomical variations in the eye.
Age is a big risk factor in the development of POAG, genetics also plays a part. If any family member has had POAG this can also increase the chances of an individual developing the disease. Other than age, genetics, and family history, people with hypertension, diabetes, race (African American), and higher than normal intraocular pressure are all at higher risk of developing the disease.
Development and Diagnosis
For anatomical narrow angle glaucoma, the diagnosis occurs promptly because of the often acute symptoms. The diagnosis includes a comprehensive eye examination that is made up of three components. The components of the eye examination include:
The first is primary open-angle glaucoma (POAG). POAG is the more common of the two types, and it progresses slowly. Often, people do not think they have it because they don’t even know their optic nerve is being damaged. It is usually detected during routine eye exams. Diagnosis to see if a patient has POAG usually includes a test that measures the intraocular pressure (tonometry), observation of the optic nerve, and a test that is designed to detect any loss in peripheral vision (visual field test).
Approach:
Solutions to anatomically narrow angle glaucoma can include medications taken with the end result being decreased intraocular pressure. Laser therapy may be used and is denoted by the use of a laser peripheral iridotomy to cut a hole in the peripheral iris in order to let the fluid drain out of the eye. The final solution may be surgical intervention of the eye where this is a procedure where the systems and tools known as gonioscopy are utilized to probe the eyes for answers and counterattack the specific issues found.
POAG: The primary therapy for POAG is directed at lowering eye pressure. This can be done with medications, laser therapy (Selective Laser Trabeculoplasty), or surgery (trabeculectomy or minimally invasive glaucoma surgery).
Healthcare professionals must understand the differences between anatomical narrow angle glaucoma and primary open-angle glaucoma in order to develop and execute the right treatment plan for the individual patient, given the right set of conditions. Regular eye exams will continue to play a significant role in the early detection and treatment of both anatomical narrow angle glaucoma and primary open-angle glaucoma.
Conclusion
There are many different aspects of anatomical narrow angle glaucoma that should be understood. This guide has addressed things such as what anatomical narrow angle glaucoma is, and what causes it to happen. You were also able to see what symptoms we were trying to treat, as well as the diagnosis we were hoping to give you. The different surgical methods are addressed as well as things to look out for after you have had the surgery. We hope that this guide has better equipped you with the necessary information to talk with your doctor before being diagnosed.
FAQ’s
What sets anatomical narrow angle glaucoma apart from other types of glaucoma?
Anatomic narrow angle glaucoma is different from other types of glaucoma in that it has to do with the physical structure of the drainage system of the eye that’s not doing its work properly. It takes the shape of a narrow angle between the iris and the cornea. It causes the fluid in the eye to be drained out with more difficulty and will eventually cause an increase in intraocular pressure.
What can be done to prevent anatomical narrow angle glaucoma?
Some risk factors of anatomical narrow angle glaucoma such as race, age, family history, and gender cannot be prevented. But there are some lifestyle choices that may considered to reduce one’s risk of suffering from anatomical narrow angle glaucoma which are taking medications for eye problems, eating a healthy diet rich in vitamins C and E, and minerals such as zinc and copper can also help. Often good nutrition can help reduce neovascularization. Getting regular eye examinations can push the limits of how far anatomical narrow angle glaucoma has progressed, and hence help save any further damage.
Can changes in lifestyle help with the management of anatomical narrow angle glaucoma?
Many patients feel that if they live a healthier lifestyle will help manage their anatomical narrow angle glaucoma. Living a healthier lifestyle that includes regular exercise, a well-balanced diet, and taking all of the medications that the doctor has prescribed for you, will help patients in the overall management of anatomical narrow angle glaucoma. Patients should be cautious of certain activities that any increase the pressure in their eyes.
The surgical options for anatomically narrow angle glaucoma are laser peripheral iridotomy (LPI) and laser iridoplasty. Laser peripheral iridotomy (LPI) is a procedure in which a hole is made in the peripheral iris allowing better drainage, Laser iridoplasty is performed by creating an opening in the peripheral iris that flattens it, decreasing the angle. The surgery option chosen is individual to each person based on severity and personal. Surgical options are effective but success is dependent on the individual.
Does narrow angle glaucoma run in families?
Defining the Role of Genetics in the Family History of Consideration has been given to genetics of narrow- angle glaucoma. That is, the genetic component for the incidence of primary angle closure glaucoma may be higher in people of Asian descent than in other racial groups due to an increase in the thickness of the anterior or frontal part of the eye in people of Asian descent. Also, people with a family history of glaucoma may be at a higher risk for angle glaucoma. Nonetheless, the role of genetics may be extremely complex due to determining which of the many genes are associated with the development of narrow-angle glaucoma.