AMD progression can be reduced through healthy eating habits, keeping out of direct sunlight by wearing protective eyewear such as sunglasses and hats, not smoking and scheduling regular eye exams – in addition to recent advances in treating wet macular degeneration.
Treatment for wet AMD typically entails injecting drugs that prevent abnormal blood vessel growth in your macula. Such medications can protect vision in early stages of wet AMD.
Wet AMD
Wet AMD (also referred to as Neovascular or Exudative AMD) occurs when abnormal blood vessels form beneath the retina and begin leaking blood and fluid into layers of the eye, damaging central vision and making contrast more difficult to see. It’s usually more serious than dry AMD and can even lead to blindness within weeks if left untreated adequately; those with family histories of wet AMD are at a greater risk. Smokers also are at increased risk. Wet AMD tends to affect people more severely.
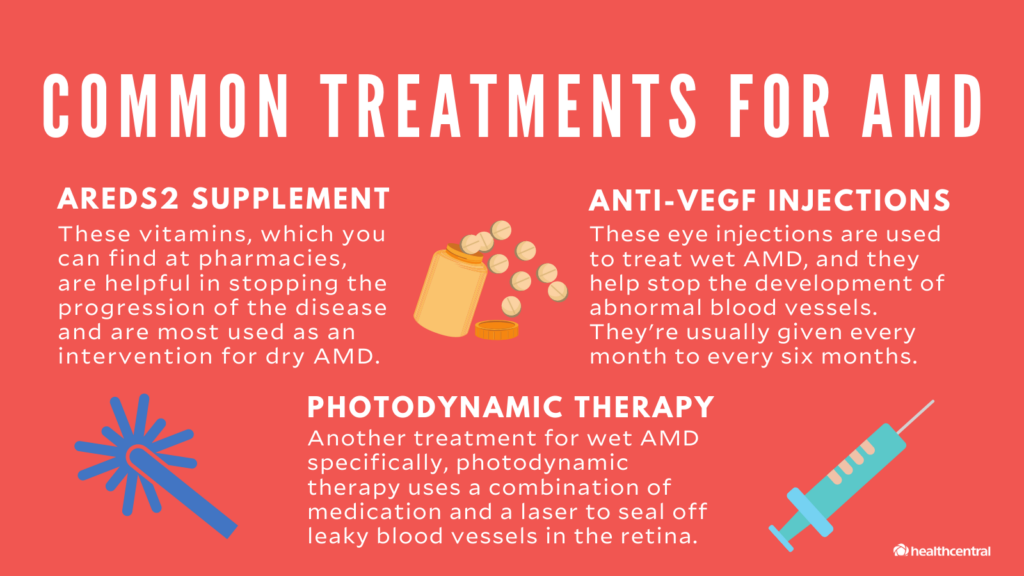
Treatment for wet AMD involves injecting anti-vascular endothelial growth factor (anti-VEGF) medicines directly into the eye. These work by blocking proteins or pathways responsible for abnormal blood vessel growth; however, regular treatment visits must still occur to be effective; new drugs are being developed which may help decrease their frequency.
Four commonly prescribed anti-VEGF drugs, all administered intravitreally via an injection procedure called an intravitreal injection, are available. Three of them – ranibizumab (Lucentis), aflibercept (Eylea) and brolucizumab (Beovu) were specifically designed to treat wet AMD; bevacizumab (Avastin), designed for other conditions but increasingly being prescribed for wet AMD “off-label.”
All these drugs are highly effective and safe when taken as directed, with up to 95% chance of preventing severe vision loss and up to 40-44% of recovering much of what had been lost through treatment.
Costs associated with treatments like photodynamic therapy (PDT) can be substantial; however, most insurers or Medicare will cover them. PDT involves giving a dose of numbing medication before shining light over both eyes to release light-sensitive drugs that travel throughout your body and stick only to damaged blood vessels before being destroyed with laser technology.
Early wet AMD may not warrant treatment as the abnormal blood vessels tend to settle without intervention. NHS guidelines advise monitoring such patients closely, only acting if their vision worsens significantly.
Dry AMD
Dry AMD occurs when small deposits known as drusen form under the retina. It’s thought these are caused by blood vessels’ inability to efficiently clear away waste produced by retinal cells; over time they build up, potentially creating visual distortion and distorting vision in some small areas. People living with dry AMD are at a greater risk for wet AMD which can quickly lead to blindness.
Wet AMD occurs when new blood vessels form under the retina and scar its retinal pigment epithelium (RPE). They may also leak fluid into RPE and damage photoreceptors; additionally, this fluid may obstruct signals between retina and brain and ultimately cause central vision loss as well as color perception issues. Both types can lead to vision loss.
Scientists are working tirelessly to develop treatments that slow or reverse the progression of dry AMD. One such medication, known as a Sigma-2 antagonist, works by blocking an action taken by molecules which promote new blood vessel growth within eyes. If taken regularly it could slow disease progression by up to 1-3 months annually but cannot undo damage done to vision, nor restore lost sight as there is no known cure for AMD.
Other approaches involve blocking specific proteins to mitigate oxidative stress in the eye. Animal studies have demonstrated how drugs that block their activity were successful at preventing RPE cell death – providing another step toward developing clinical therapies for dry AMD.
Stem cells could provide an innovative treatment option for dry AMD by replacing damaged RPE and photoreceptor cells, helping restore light processing ability and produce clear images in the eye.
Researchers continue to advance treatments for wet and dry AMD while exploring their fundamental biology. One recent study discovered that HIF-1 controls an eye’s response to oxidative stress, contributing both wet and dry AMD by protecting against it while simultaneously contributing to it as well. If HIF-1 is overactivated too frequently it could promote wet AMD just like it protects against dry AMD.
Diagnosis
AMD affects the central part of your vision, making it hard to read, drive a car or recognize faces. While AMD progresses over time, treatment and management can help slow its deterioration and limit further vision loss. Regular visits to your eye doctor as well as monitoring yourself at home with an Amsler grid may help. These grids consist of straight horizontal and vertical lines which you should observe every day to detect wavy or broken lines that need medical attention immediately if noticed distorted. If this is happening immediately call your eye doctor immediately
As part of your eye exam, tests such as optical coherence tomography (OCT), which creates cross-sectional images of your retina, can detect buildup of drusen and breakdown of light-sensitive cells in your eyes. Your doctor will inject yellow dye into your arm before taking multiple photos showing blood vessel outlines with color. Fluorescein angiography may also be utilized; in which an eye care professional injects the same yellow dye and takes pictures as it lights up on your retina–this can show any fluid leakage from abnormal blood vessels under macula.
If you have wet AMD, photocoagulation (a laser treatment used to destroy leaky blood vessels) may help. Although photocoagulation poses low risks of complications and growth back of blood vessels may result in further vision loss, it is important to discuss all risks with your physician prior to proceeding with surgery.
Even if your wet AMD is advanced, a healthy lifestyle and taking supplements may reduce the risk of further vision loss. Quit smoking, consume a diet rich in leafy green vegetables, exercise regularly and wear sunglasses; additionally vitamin A supplements may be useful; speak to your eye doctor about them as soon as possible to see whether or not they’re right for you.
Treatment
At Slingsby & Huot Eye Associates, we recognize there are effective strategies available to you for slowing or stopping dry AMD in its tracks. A regular screening with our macular degeneration specialists at Slingsby & Huot can detect any early symptoms before they cause vision loss; vitamins, supplements and diet can also help slow progression of this common condition.
Late stage AMD (known as exudative or neovascular AMD), in which abnormal blood vessels form beneath the retina, causes leakage of fluid and blood into the macula and may result in severe vision loss or blindness over time. While rarer than its dry counterpart, exudative AMD is caused by similar factors including ageing, family history of disease, smoking habits and sun exposure.
Research has demonstrated that certain genes, like the ARMS2 gene and its homolog, can increase your risk for wet AMD. Furthermore, other factors like smoking, obesity and diet also play a crucial role.
Treatment for wet AMD typically entails using both medications and laser photocoagulation to address leaky blood vessels and stop further leakage. Your doctor may also suggest fluorescein angiography – injecting dye into an arm vein before taking pictures of your retina as the dye highlights its blood vessels – for best results.
Optic coherence tomography (OCT) uses dim lighting to produce cross-sectional images of both eyes and retinas, enabling doctors to easily detect any thinned out or misshaped retinal layers as well as new abnormal blood vessels in the eye.
Intravitreal injections of medicine into the eye are the best solution to treating wet AMD, and should be administered monthly without pain or side effects. Anti-VEGF therapy involves blocking harmful signals that promote abnormal blood vessel growth under the retina – popular anti-VEGF drugs include Eylea, Bevacizumab (Avastin) and Brolucizumab (Beovu). Studies are being done with faricimab-svoa (Vabysmo), which blocks both VEGF and angiopoietin-2 (Ang-2). While treatments cannot restore lost vision they may prevent further visual loss by stopping further vision loss from progressing further down.