Macular degeneration typically causes gradual vision loss over time, though some individuals develop the wet form when abnormal blood vessels grow behind the macula and release fluid.
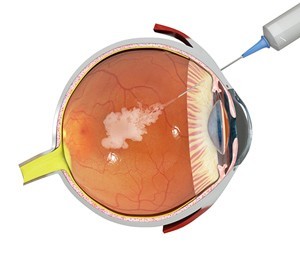
VRMNY provides two medications designed to prevent wet macular degeneration and restore vision: Lucentis and Eylea (VEGF inhibitors) which provide monthly injections of protection.
Fluorescein Angiogram
Fluorescein angiogram (FA) exams allow your eye doctor to see behind your eye with clarity. A small dose of safe dye is injected into a vein in your arm and pictures taken as it travels through your eye – this allows them to detect abnormal blood vessels growing underneath the retina as well as identify any leakage of blood or swelling of macula or retina.
Age-related macular degeneration, more commonly referred to as macular degeneration, refers to the gradual degeneration of your retina’s light sensitive tissue known as the macula. As macula function declines, blurry and distorted vision emerges, making it difficult for you to read, drive and recognize faces even though peripheral (side) vision remains normal. A wet form of macular degeneration occurs when abnormal blood vessels proliferate and leak fluid underneath your retina resulting in rapid and severe vision loss.
Your eye doctor can recommend treatment for dry age-related macular degeneration that slows its progression by slowing geographic atrophy – the yellow deposits known as drusen that form at the center of the macula – by giving regular high doses of antioxidant vitamins and zinc (recommended by the second Age-Related Macular Degeneration Study), along with other supplements like lutein, omega 3 fatty acids, or other nutrients; such supplements have proven successful at slowing advanced dry macular degeneration by roughly 20% over two years.
If you have wet AMD, your eye doctor may suggest laser photocoagulation to treat the abnormal blood vessels causing wet macular degeneration. Laser photocoagulation uses laser light energy to destroy abnormal vessels that have grown underneath your retina – this procedure works best if these abnormal vessels cluster closely together rather than being located centrally within the macula.
Though there is no cure for wet age-related macular degeneration, treating it early with laser photocoagulation can significantly lower your risk of further vision loss and in some cases even restore lost sight. Meanwhile, treatments for dry age-related macular degeneration tend to be less effective at stopping vision loss but still allow you to carry on doing the tasks you enjoy without interruption.
Amsler Grid Test
The Amsler Grid Test is a self-assessment tool that enables people to monitor changes in their vision. This tool is particularly beneficial for people living with wet (neovascular) AMD as it helps detect early symptoms that might require treatment – potentially helping avoid further central vision loss.
It is easy to use, and people with AMD should use it regularly as part of their self-care regime. People over 55 at risk of AMD should also participate, since early diagnosis may help spot potential issues before they worsen, alerting eye healthcare professionals of additional tests being necessary.
An Amsler grid should produce straight and uniform lines and squares when looking through healthy eyes, and any deviation can indicate macular degeneration or another central vision disorder. Blank or dark areas may indicate leakage from blood vessels under the retina.
An Amsler grid should be used in a well-lit room and glasses wearers should put them on before beginning the test. It is best to do the examination one eye at a time as this helps detect problems more accurately. Regular use is encouraged as using it every day can identify changes in vision. Patients should contact their eye doctor if any sudden or noticeable changes arise in vision.
Those noticing irregularities on their Amsler grid should seek medical advice immediately if it appears wavy, broken or distorted – as these symptoms could indicate wet AMD which can be more difficult to treat and lead to rapid vision loss.
Patients living with wet AMD can benefit from various treatments, including injections of anti-VEGF medication or photodynamic therapy, which may slow its progress and preserve quality vision in many instances. Unfortunately, such therapies are only available during early stages of wet AMD development, so early intervention is key in order to preserve sight.
Visual Field Test
A visual field test measures peripheral (side) vision, which helps you see things around you. This eye map displays which areas are clear to see while others might appear blurry, wavy or dark – an invaluable way of detecting glaucoma and other conditions that damage retinal nerves and result in vision loss as well as tracking treatment progress over time.
Visual field tests come in many varieties. From quick screening tests that can be conducted during an eye exam – like Amsler grid perimetry – to more extensive computerized exams such as Goldmann perimetry. Both require patients to keep their gaze fixed on one central point for extended periods, cooperating fully with their technician so as to obtain reliable results.
To conduct a visual field test, the doctor first applies eye drops to both eyes, then numbs them using a speculum. A technician will then move test probes around your eyes until you see flashes of light in various test areas; at these moments you are required to press a button each time one appears; this tells the computer which areas of vision have been tested, which compares it against similar tests conducted by people from your age and gender demographic. If any results indicate significant loss in vision this could indicate glaucoma; in which case your eye doctor can use this test results information in helping make decisions regarding treatment plan decisions.
Visual field testing can also detect “blind spots,” also known as scotomas or “blind areas.” Scotomas are areas in the visual field where objects cannot be seen – one of the first signs of glaucoma. Understanding its type and size helps your eye doctor pinpoint any causes for vision loss such as glaucoma or other factors like drooping eyelids (ptosis). Annual visual field tests typically come covered by vision insurance for those diagnosed with glaucoma or other ocular diseases.
Drusen Test
Drusen are one of the telltale signs of age-related macular degeneration in its dry form: yellow or white deposits underneath the retina that, over time, lead to macular thinning, distortion, and eventually the loss of central vision. Drusen are usually painless in early stages; should they expand larger however, you may need to monitor for changes to your vision by visiting an eye doctor regularly.
Many drusen are easily visible during an eye exam, yet those buried near the optic nerve head may prove more challenging for your eye doctor to diagnose due to appearing as swelling of the optic nerve itself – something which could misdiagnose as serious conditions like papilledema (caused by high pressure and swelling in the brain) leading to misdiagnosis of severe conditions like papilledema which require hospitalization for neuroimaging and lumbar puncture procedures along with treatments of steroids and fluids in order to prevent permanent vision loss.
Drusen formation may not be fully understood, yet evidence exists to suggest they could be an early indicator of central retinal artery occlusion (CRAO). CRAO occurs when small blood vessels in the back of the eye form abnormal connections with surrounding tissues which leads to bleeding; it can occur as a result of systemic hypertension, migraine headaches, oral contraceptive use or smoking among others.
Drusen may be an early indicator of wet macular degeneration (AMD), an advanced form that rapidly leads to vision loss. Wet AMD is marked by abnormal blood vessel growth under the retina that leak blood and fluid into the macula, leading to blurry vision, distorted straight lines, blind spots and other symptoms of damage in its wake. People who smoke regularly and have had cataract surgery are especially susceptible to developing it as it increases with each subsequent generation.
Macular degeneration cannot be cured, but treatment options include nutritional supplements, laser treatments and/or medication prescribed by eye doctors. Furthermore, adhering to their instructions for monitoring and treatment will decrease your risk of progression from dry macular degeneration into wet type macular degeneration.