Indications for treatment include 20 / 40 vision due to macular edema and neovascularization; occult telangiectasis with yellow exudates located 1-2 disc diameters temporally from fovea; and an abnormal Ophthalmoscopy examination;
Sudden onset of vascular obstruction with retinal vein occlusion, capillary closure and retinal hypoxia; visual acuity gradually declines from count fingers to light perception; often associated with cherry-red spots.
Visual Acuity
Visual Acuity measures one’s ability to recognize black symbols (optotypes) against a white background at a set distance – often letters, numbers or shapes such as letters. Visual acuity is often the first telltale sign of eye disease because it measures central vision directly.
Eye care providers use the Snellen chart to measure visual acuity in patients. Patients must read each line starting with the largest letters before gradually working their way down towards smaller ones until they reach 20/20 vision status.
Not only is visual acuity measured, but other components of an eye’s ability to process fine detail are as well, including color perception, pupillary reflexes and Golmann visual fields. These tests may help diagnose eye disorders such as ptosis, cataracts and strabismus.
Though these tests can be helpful, they may not accurately reflect a patient’s best-corrected visual acuity. A recent study published in VEHSS showed that self-reported visual acuity survey questions vary considerably among individuals and are only moderately related to prevalence estimates based on best-corrected visual acuity estimates.
When evidence of hypertensive retinopathy exists in a patient, initial examination should focus on visual acuity and pupil dilation. When administered during examinations of hypertensive patients, however, eye exams are especially crucial as failure to cooperate can make valid measurement difficult; sleepy or intoxicated patients might fail to recognize optotypes correctly leading to underestimation of visual acuity measurements.
Keep in mind, however, that visual acuity may also be affected by other issues, including reduced contrast or inability to track fast-moving objects. Therefore, using the Snellen chart alone should not serve as an accurate measurement of a person’s ability to perceive fine details; other evaluation tools, including color and visual field tests should be employed as well for more comprehensive testing results.
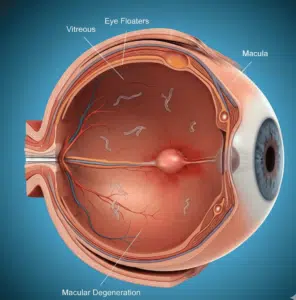
Ophthalmoscopy
Eyes provide a window into our overall health, with hypertension, diabetes, and cardiovascular disease often manifesting themselves through changes to eye blood vessels. Primary care physicians with an ophthalmoscope can quickly spot these telltale signs early on for early intervention and holistic patient care.
Ophthalmoscopy is a method for inspecting the eye and retina (light sensitive layer at the back of your eye) using a special torch-like instrument known as an ophthalmoscope. Small drops are placed into each eye to dilate (open up) its pupil before light is shone through an ophthalmoscope onto your retina – this process generally only takes several minutes without causing pain or discomfort to either party involved.
Retroillumination allows the examiner to carefully inspect all aspects of retina (tapetum, non-tapetum, blood vessels and optic disc) while patient holds their chin up on a brow rest. Care is taken in aligning condensing lens parallel with iris while maintaining condensing lens axis with pupil axis so as to keep constant tapetal reflection. Furthermore, peripheral retina for any signs of thinning, hemorrhage, leakage or RPE atrophy should also be evaluated by using retroillumination.
Examiners must remain wary of ocular trauma that can result in retinal hemorrhage and loss of vision, usually after experiencing blunt trauma. Rupture sites tend to be circular or concentric to the optic nerve, although crescent-shaped or hemicortical rupture sites may occur as well; usually though, hemorrhage obscures this rupture site and it becomes inaccessible; rupture in the macula requires extensive treatment efforts with poor prognosis; however if only peripheral retina is affected, vision should return once healed after it heals over time.
After retinal hemorrhages have healed, choroidal neovascularization (CNV) often appears. CNV can be recognized by its scattering of ovoid hyporeflective spaces across retinal pigment epithelium (RPE). Its presence suggests capillary leakage from newly formed neovascularizations while yellow or blue hued sclera indicates peripheral edema or neovascularizations affecting peripheries; these areas may benefit from laser photocoagulation or use of anti-VEGF agents to treat these areas and possibly improve vision.
Fluorescein Angiography
Fluorescein angiography is a diagnostic test that allows doctors to visualize blood circulation within the eye. This helps doctors accurately diagnose retinal conditions like hypertensive retinopathy and age-related macular degeneration. Tracking patient progress and monitoring treatment. A small amount of orange-red dye is injected into the patient’s arm, then their doctor takes pictures (angiograms) using a special camera of inside of their eye using special lighting – painlessly and safely. Some side effects from injection may include nausea or headache that will subside after several minutes, though a small minority are allergic to the dye and may experience skin rash, vomiting and more severe headaches as a result of taking it; but this is very uncommon. Please bring a list of medications you take – both prescribed and over-the-counter drugs or supplements – when coming for your appointment.
An angiogram is an imaging technique used to detect leakages or blockages in blood vessels of the retina and choroid. Dye is injected into a vein in the patient’s arm and traveled directly into their bloodstream until reaching retinal vessels, where images were then captured and evaluated by doctors. This test can identify location, size, shape and pattern of filling and leakage of retinal blood vessels as well as disease such as Choroidal Neovascular Membranes (CNVs), Macular Edema or Diabetic Retinopathy.
Angiograms may be recommended by doctors for patients exhibiting symptoms including sudden vision loss, increased glare or halos around lights and blurry or dark areas in the center of their visual field (macular edema). An angiogram is especially helpful in diagnosing CNV, macular edema and other diabetic-related eye diseases that could eventually lead to blindness; additionally it can also determine if certain treatments such as laser photocoagulation or anti-VEGF agents are working effectively.
This vascular disorder is characterized by the formation of new blood vessels under the retina that leak fluid, leading to loss of focused central vision that interferes with reading, driving, and other activities. Other symptoms may include headache, vision distortion, color distortion and increased pressure in the eye. An angiogram can identify new blood vessels present and help a physician decide upon appropriate treatment plans for each individual patient.
Optical Coherence Tomography
Optical coherence tomography (OCT) is an imaging study used to measure retinal layer thicknesses. Similar to ultrasound but using light rather than sound waves, OCT provides invaluable information regarding patient retinal health as well as monitoring treatment responses and can even predict future needs based on its measurement results. You may receive OCT at each visit or more frequently if your condition worsens.
Optic coherence tomography allows your doctor to visualize each layer of your retina in great detail, showing its thickness as well as any changes or progression. It is an invaluable way of diagnosing hypertensive retinopathy and diabetic macular edema.
OCT testing can assist your doctor in predicting how long it will take for macular edema to subside when treated with laser therapy or anti-VEGF injections, or determine if you need additional therapies such as triamcinolone injections. Furthermore, this noninvasive test won’t cause any discomfort to you or anyone around you.
If you experience a severe eye bleed or hemorrhage, it’s imperative that you contact your physician immediately. Otherwise, the retinal artery could become compressed, leading to permanent vision loss caused by fluid from behind-the-retina bleeding or by blood vessel rupture – the first sign may be sudden loss of vision or distortion in your central field.
Other symptoms may include gray-white discolorations of the retina known as Berlin’s whitening; caused by intracellular edema and disorganization of outer retinal layer. While it can affect any part of retina, macula areas tend to be affected most commonly and it is accompanied by hemorrhages or rupture.
Fluorescein angiograms can provide useful diagnostic data that reveals delayed retinal vein filling, prolonged transit time and extensive capillary nonperfusion (defined by CVOS as >= 10 disc areas of capillary nonperfusion), staining of vascular walls and blocking defects. A wide-field fluorescein angiogram is generally advised after extensive capillary nonperfusion and staining is observed as well as staining on arterial walls due to blockages; an electrophysiologic testing study of the eye (reduced b wave amplitude with reduced a-wave amplitude as an indication of ischemia), electrophysiologic testing study of normal atrophy) along with medical consultation for comprehensive cardiovascular evaluation should follow immediately after being detected by wide-field fluorescein angiogram.