What are narrow angles in the eyes?
A “narrow angle” describes the shape of the eye’s drainage angle. People who are farsighted tend to have narrow angles. People who are farsighted have shorter eyes than people who are nearsighted.
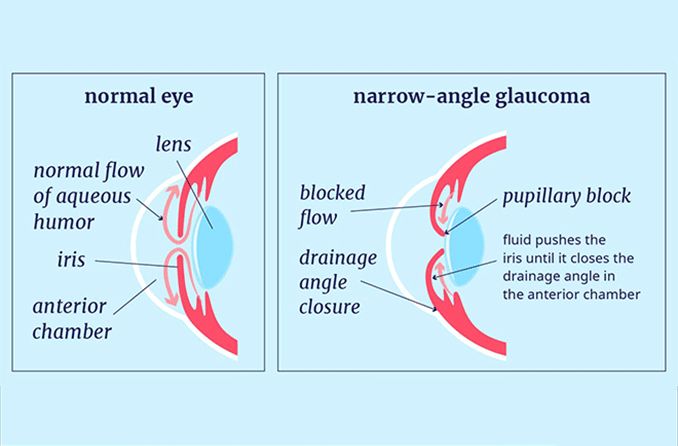
There may not be enough space in front of the eye for both the lens and the iris if the eye is shorter. The bright part of the eye is called the iris. This can make things crowded, which can push the iris toward the clear part of the eye called the cornea. The cornea is the front part of the eye that is clear. Between the lens and the iris is where the eye drains.
If the iris is pushed forward, it can block the drain. An angle closure event could happen to you because of this.
There aren’t many people who have narrow-angle glaucoma, and it’s not like open-angle glaucoma in that the eye pressure gets very high very quickly. This takes place when the drainage tubes get clogged or covered up. As the iris hits the lens of the eye, the drainage angle closes off. The lens and the iris can stick together sometimes. This causes the pressure to rise quickly, generally in one eye. Along with redness, swelling, and blurred vision, the eye may feel a sensation of pressure.
Who is at risk for a narrow angle eye?
Most people with narrow angles are hyperopic, which means they are “farsighted.” Most of the time, these are people who have never needed glasses to see clearly, except for reading glasses after age 40 or so. People with hyperopia tend to have shorter, smaller eyes than most people. This makes the eye smaller and more compressed, including the angle. People who are nearsighted or farsighted and over 65 who have not had cataract surgery are also at risk. This is because as a cataract grows, it pushes the eye forward, which makes the angle smaller.
What signs does a narrow angle eye show?
Usually, narrow angles don’t cause any symptoms, which means the patient doesn’t notice they are there. At the same time, angle closure can cause severe symptoms like headaches, blurred vision, nausea, vomiting, redness, and intense eye pain if it happens. Angle closure attacks can happen to people with narrow angles from time to time. These attacks are generally accompanied by a mild to moderate headache in low light, blurred vision for a few hours, redness, and sometimes nausea and vomiting.
What is glaucoma exactly?
Glaucoma is an eye disease that damages the optic nerve, which sends messages from the eye to the brain about what the eye sees. This damage leads to vision loss.
Most cases of glaucoma happen when there is high intraocular pressure (IOP) inside the eye. This is because fluid tends to build up and not drain properly.
Glaucoma is known for stealing one’s sight slowly without any symptoms.
What does angle-closure glaucoma mean?
Angle closure glaucoma happens when the eye’s drain gets clogged, which makes the pressure inside the eye rise. The iris is pushed forward inside the eye, which blocks the drainage angle. The name for this is acute angle-closure glaucoma if it happens quickly. With severe angle-closure glaucoma, you can lose your sight if you don’t see an eye doctor right away.
When the eye’s drainage angle is closed slowly, the pressure builds up over a longer time. We call this long-term angle-closure glaucoma. You can also lose your sight if your eye doctor doesn’t handle chronic angle-closure glaucoma.
Both types of angle closure glaucoma are more likely to happen if your angles are small.
What makes narrow-angle glaucoma happen?
When the iris, the colored part of the eye that covers the pupil, bows forward, it makes the drainage angle between the cornea and the iris smaller. This is what causes narrow-angle glaucoma.
There is a link between narrow-angle glaucoma and these things:
Plateau Iris
A disease where the ciliary body is too far forward in the eye. The ciliary body is the structure behind the iris that makes the aqueous fluid in the eye.
The peripheral iris is pushed forward, which makes the drainage angle smaller and makes it more likely that the front area of the peripheral iris will block the eye.
Tumors and other reasons
Long-term angle-closure glaucoma can also be caused by a growth behind the iris, swelling from ciliary body inflammation (intermediate uveitis), or changes in the eye’s structure after surgery for a retinal detachment.
A person should be checked for glaucoma regularly but at least twice, once around age 35 and again around age 40. People who are more likely to get narrow-angle glaucoma should have their pressure checked once or twice a year. This includes Asians, people who are farsighted, and people over the age of 60.
Because narrow-angle glaucoma can have very bad effects very quickly, you should see an eye doctor right away if you have any of the above symptoms.
To measure your eye pressure, your doctor will use tonometry when they check your eyes. The tonometer is gently pressed against the eye after numbing drops are put in it. The resistance is measured and written down.
To find out if you are likely to get narrow-angle glaucoma, the angle structure of the eye is looked at under a microscope. This is important because there are ways to treat the problem before it gets worse.
You can look at the shape and color of your optic nerve with an ophthalmoscope. The ophthalmoscope makes the inside of the eye look bigger and brighter. More tests will be done if the optic nerve looks like it’s been impacted or isn’t a healthy pink color.
A key difference between open-angle glaucoma and narrow-angle glaucoma is whether the angle where the eye meets the cornea is open or closed. Gonioscopy can tell you if this angle is open or closed.
How common is glaucoma with a narrow-angle in the eyes?
Different racial groups have different rates of narrow angle myopia. It is very uncommon in white people; only 3.8% of white people in the US are thought to have it. People with East Asian roots are much more likely to have it, especially those from Thailand, Myanmar, and China.
A lot of white people with glaucoma have open angle glaucoma. About nine out of ten cases of glaucoma in Asian people are narrow angle.
For both acute and chronic narrow angle glaucoma, Inuit people and women are more likely to have them.
How bad is narrow angle eye glaucoma?
Narrow angle glaucoma can make it very hard to see. There aren’t as many cases of narrow angle glaucoma as there are of open angle glaucoma, but it still causes half of all blindness cases.
If someone with acute or chronic narrow angle glaucoma doesn’t get care, they can lose their sight for good. Because the acute form comes on quickly, it can change your vision within hours.
How are narrow eye angles treated?
“Like open-angle glaucoma, angle-closure glaucoma comes in many forms,” says Jeffrey M. Liebmann, MD, clinical professor of ophthalmology at New York University School of Medicine, adjunct professor of clinical ophthalmology at New York Medical College, and director of glaucoma services at New York University Medical Center and Manhattan Eye, Ear, and Throat Hospital. Anatomically narrow angles, angle closure, and acute angle-closure attacks are not just caused by one disorder. They are caused by a number of different diseases. Because of this, the most important thing doctors can do for angle-closure glaucoma is to try to find the reason for the closure by following a set of steps, just like they would for primary open-angle glaucoma. It’s possible to treat something if you know what caused it.
Not every narrow angle of the eye needs to be fixed. In some cases, your eye doctor may not think you are at high risk for an acute angle closure attack. They will just keep an eye on your eye.
At other times, your angles are so small that you have a high chance of having an acute angle closure attack. Most of the time, your eye doctor will suggest a laser procedure called a laser peripheral iridotomy.
To stop an acute angle closure attack, this laser makes a hole in your eye that lets fluid out. If there is too much fluid in your eye, it is possible for it to drain without making your eye pressure rise too high.
The laser cuts a small hole in the eye. After the laser hole, also known as a laser peripheral iridotomy, you won’t have an acute attack because your iris won’t be able to fully block your drain.
If your eye doctor has told you to get laser treatment, you should stay away from things that will make your pupil bigger before the treatment. The eye tissue bunches up even more inside the drain when your pupil gets bigger. This could lead to a severe attack.
Over-the-counter medicines for colds and some medicines for motion sickness can make the pupils bigger. These shouldn’t be taken until after the laser treatment. You should carefully read the labels on all new prescription and over-the-counter medicines. If it says not to take it if you have glaucoma, then don’t. (You are at risk for the type of glaucoma they are telling you about.)
Preventing damage from narrow angles in the eye
At the moment, lowering the IOP to a level at or below a clinician-set goal that is specific for each patient is the only proven way to stop glaucoma damage from getting worse. As you work toward your goal, remember that IOP changes naturally from day to day and from hour to hour during the day.
Different eyedrops (rarely pills), laser treatments, and surgery are all possible solutions. As an initial treatment, eyedrops and laser may work just as well, but in the US, most people choose eyedrops because they work well, don’t have any side effects, are easy to use, and are becoming more and more affordable. Elderly people, on the other hand, may find it hard to stick to treatment plans that last a lifetime. Costs depend on the patient’s insurance, but if they pay for two or three drugs out of pocket every month, it could cost $200.
In laser trabeculoplasty, the laser is used to change the draining angle, which speeds up the flow of fluid out of the body. The process is simple and doesn’t hurt. It’s usually done in an office setting. Over time, the benefit might wear off, so patients still need to be closely watched.
When eyedrops, lasers, or both aren’t helping and the patient’s condition is getting worse, an ophthalmologist may suggest surgery to make a new way for fluid to drain. A trabeculectomy or, if that doesn’t work, a tube shunt may be needed.
At what point should I see a doctor?
If you are farsighted, you should get your eyes checked once a year to make sure you aren’t developing a narrow angle. If you have any of the other symptoms listed above—headaches that hurt more in dim light, blurry vision that comes and goes, eye pain, or redness—you need to see a doctor right away. You can make an appointment with an eye doctor to help you figure out what might be wrong.
In conclusion
True glaucoma avoidance is possible in narrow angle eye disease with laser iridotomy, some cases of trauma-related glaucoma by wearing face shields for certain sports, and steroid-induced glaucoma by stopping steroids. In general, though, we can’t stop glaucoma.
We can’t stress enough how important it is to get regular eye examinations. We probably won’t be able to stop the disease from getting worse even with care. We can slow it down, though, by lowering the IOP. Patients who are willing to make changes can and do slow down the disease enough so that they can live without losing their sight.