AMD (age-related macular degeneration) and DR (Diabetic Retinopathy) are the most common retinal conditions, and the DME (Diabetic Macular Edema) group may be regarded as a progression of DR throughout the course of the disorders.
Macular Degeneration
Macular degeneration, commonly known as age-related macular degeneration (AMD), is the major cause of visual loss in those over the age of 50. The macula, the region of the retina responsible for the sharp, detailed center vision required for reading or driving, is affected by macular degeneration. The tissue in the eye that is responsible for vision tends to degrade as we age, which may have a substantial impact on a patient’s quality of life.
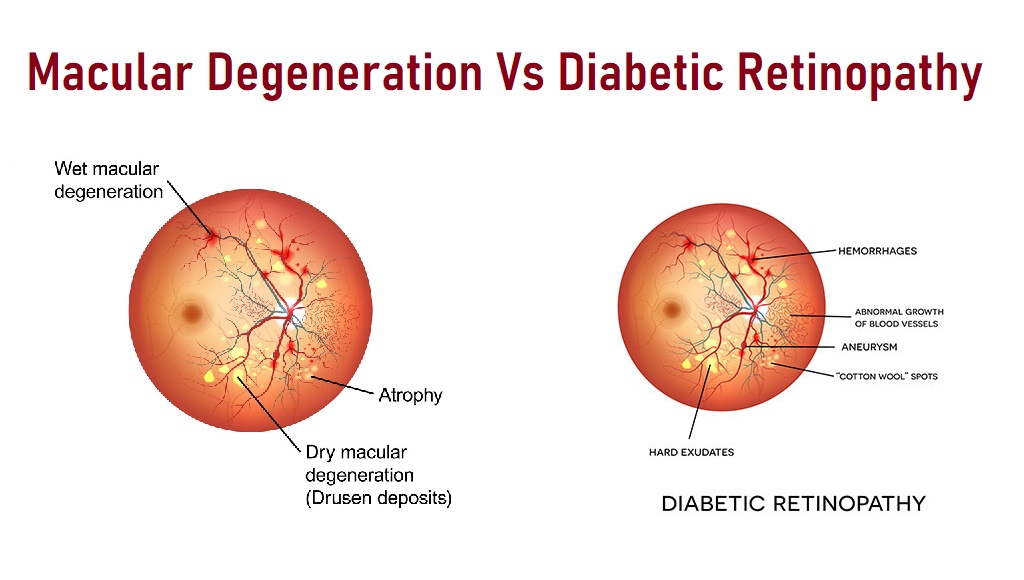
AMD, like DME (Diabetic Macular Edema), is a retinal ailment characterized by the formation of drusen deposits in the early stages of the illness, known as dry AMD. Drusen disturb the way the eye works when the condition develops to wet AMD, causing new and irregular blood vessels to emerge. Vision distortions, blurring, and difficulties seeing things immediately in front of you are all symptoms of this condition. Wet AMD may lead to permanent visual loss if left untreated.
Types of AMD
Dry macular degeneration
The majority of patients (about 90%) suffer a kind of AMD known as “atrophic” or “dry” AMD, which occurs as the macula tissues weaken with age. Dry AMD often results in a gradual loss of eyesight. Drusen deposits are seen in this kind.
Wet macular degeneration
A lower percentage of patients (about 10%) experience a more problematic disease known as “exudative” or “wet” AMD when irregular blood vessels develop behind the retina. Blood and fluid escape from these diseased arteries, scarring the macula. Wet AMD sufferers may have quick and severe vision loss.
Diabetic Retinopathy
It is a diabetic eye disease that is caused by damage to the retina’s blood vessels. This illness is treated but not curable. It may produce no symptoms but just minor visual difficulties, or it may cause severe vision loss if left untreated. The retinal blood vessels are compromised to the point that fluid leaks out and vision is altered.
As life expectancy rises, the probability of developing age-related clinical disorders rises as well. Diabetes mellitus, a systemic illness that causes substantial impairment of various physiologic systems, including vision, up to full blindness, is one of the most frequent. The Centers for Disease Control and Prevention, in particular, presented a concerning estimate (Zhao and Singh al., 2018): diabetes affects 9.4% of the US population. More than one-third of the worldwide population with diabetes (Herat et al., 2018) is afflicted by diabetic retinopathy (DR), typically with vision-threatening DR (severe non-proliferative or proliferative DR) or diabetic macular edema (DME) (Yau et al., 2012). Furthermore, age-related macular degeneration (AMD) affects around 11 million Americans and 170 million individuals worldwide (Pennington and DeAngelis, 2016), with these numbers expected to rise to 196 million by 2020 and 288 million by 2040 (Jonas et al., 2017), owing to the extended life expectancy.
DR is one of the most frequent microvascular consequences of diabetes, with 191.0 million individuals expected to be impacted by 2030. 2018; Herat et al.
Types of Diabetic Retinopathy
NPDR (Non-proliferative diabetic retinopathy)
Non-Proliferative or Background Diabetic Retinopathy is the beginning stage where small retinal blood vessels can break and leak.
PDR (Proliferative diabetic retinopathy)
When new blood vessels form abnormally inside the retina, this is known as proliferative diabetic retinopathy (neovascularization). This new growth has the potential to produce vitreous bleeding, scarring, or retinal detachment, resulting in visual loss. Once the retina can no longer consistently absorb the fluids from those leaky blood vessels, diabetic retinopathy develops DME. The macula thickens and swells as a result of this.
The swelling might be localized or extend out across a large region. More edema usually results in more symptoms.
DME is a consequence of diabetic retinopathy, therefore if you have DME, you’ll also have diabetic retinopathy. However, diabetic retinopathy may occur without the presence of DME.
Other Diabetic retinal complications
Blood veins transport blood to and from the retina, a light-sensitive tissue at the rear of the eye. Blood from the retina is drained into the main central retinal vein and away from the eye via smaller branches of retinal veins. When one of these veins becomes clogged or obstructed, it is called a retinal vein occlusion. Sudden blurring or loss of vision in all or part of one eye are symptoms of retinal vascular disease.
Retinal vein occlusion may be divided into two categories. When the main vein of the eye gets blocked, it is known as central retinal vein occlusion (CRVO). When one of the smaller branches of the vessels gets blocked, it is known as branch retinal vein occlusion (BRVO).
When the retina is separated from its usual position, it is called a retinal detachment (RD). An RD is a medical emergency that may result in irreversible vision loss or blindness if not treated quickly. Fortunately, flashes of light, an increase in floaters, or a curtain blocking your vision are all warning signs and symptoms of retinal detachment.
Unfortunately, many individuals are unaware of the seriousness of the warning signs of retinal detachment, and they delay seeking medical help in the hopes that the symptoms would go away. In other situations, symptoms fade for a short time before severe retinal detachment causes visual loss over the following several days or weeks. Retinal detachment cannot always be effectively healed at this time, and vision loss may be permanent. It’s critical to contact an ophthalmologist as soon as you notice symptoms of retinal detachment.
Symptoms of macular degeneration vs diabetic retinopathy
As mentioned above, AMD is usually a slow deterioration and the symptoms come on slowly. They usually consist of slightly blurred vision and possibly some metamorphopsia (wavy vision). If it converts to the wet form the visual acuity will drop dramatically and for sure will be distorted.
Diabetic retinopathy for the most part doesn’t have any symptoms unless it becomes severe enough to affect the macula such as DME. At this point, the symptoms are similar to AMD and will cause central vision blur and wavy vision. If either a vein or artery occlusion occurs there is sudden and profound central or peripheral vision loss depending on what vessel is occluded.
Demographics of those most affected by macular degeneration vs diabetic retinopathy
Diabetes
For the whole population of the United States in 2018, the following rough estimations were made:
- Diabetes has been diagnosed in 26.9 million persons of all ages, accounting for 8.2 percent of the US population.
- Diabetes has been diagnosed in 210,000 children and adolescents under the age of 20 years, or 25 per 10,000 US youngsters. There are 187,000 people with type 1 diabetes among them.
- 1.4 million persons aged 20 and above, or 5.2 percent of all adults in the United States with diabetes, said they had type 1 diabetes and used insulin.
- Within a year of being diagnosed with diabetes, 2.9 million individuals aged 20 and up began taking insulin, accounting for 10.9 percent of all adults in the United States.
Age-adjusted statistics for 2017–2018 among US people aged 18 and above revealed the following:
- The greatest rates of diagnosed diabetes were seen among American Indians/Alaska Natives (14.7%), Hispanics (12.5%), and non-Hispanic blacks (11.7%), followed by non-Hispanic Asians (9.2%), and non-Hispanic whites (9.2%). (7.5 percent )
- The greatest frequency of diagnosed diabetes in women was among American Indians/Alaska Natives (14.8 percent )
- In comparison to non-Hispanic blacks (11.4%), non-Hispanic Asians (10%), and non-Hispanic whites (8.6%) males, American Indian/Alaska Native men had a considerably higher incidence of diagnosed diabetes (14.5%).
- Mexicans (14.4%) and Puerto Ricans (12.4%) had the greatest incidence rates among Hispanic adults, followed by Central/South Americans (8.3%) and Cubans (8.3%). (6.5 percent )
- Asian Indians (12.6 percent) and Filipinos (10.4 percent) had the greatest incidence rates among non-Hispanic Asians, followed by Chinese (5.6 percent ). The frequency of other Asian ethnicities was 9.9%.
- Prevalence differed greatly among adults depending on their educational degree, which is a measure of socioeconomic position. In particular, 13.3% of persons with less than a high school degree had been diagnosed with diabetes, compared to 9.7% of those with high school education and 7.5 percent of those with higher education.
According to a 2017 research, 75 percent of patients with type 1 diabetes and 50 percent of those with type 2 diabetes acquire retinopathy at some time in their life.
Macular degeneration
Per the Nation Eye Institute, white Americans account for the bulk of AMD cases. In 2010, 89 percent of AMD patients in the United States were Caucasian. Black and Hispanic Americans, on the other hand, accounted for 4 percent of AMD cases apiece.
Treatments of macular degeneration vs diabetic retinopathy
Treatment of dry AMD consists of mostly diet and monitoring. Lots of green leafy vegetables, foods low in cholesterol, and taking a good AREDS ocular vitamin. Quitting smoking is one of the most beneficial things you can do.
The treatment for wet AMD is usually a shot of an anti-VEGF medication to stop the formation of the new, fragile blood vessels. Another common treatment uses a light-activated dye that plugs the tiny vessels when activated causing them to atrophy and dyes off.
Diabetic retinopathy treatment can vary from just monitoring your blood sugars and retina with regular eye exams to Photocoagulation laser treatments for severe retinopathy with neovascularization (new blood vessel growth). Injections of the anti-VEGF are also used when there is neovascularization similar to AMD.
Conclusion
Macular degeneration and diabetic retinopathy can both be very serious eye conditions. Both usually are slow and progressive. Both can affect your central vision however diabetic retinopathy can also affect your peripheral vision. Symptoms can be similar when the central vision is affected. Diabetes affects blood vessels of the retina and AMD causes atrophy of the retina itself. Treatments can be the same if it is wet AMD and DME or PDR but vastly different if it is dry AMD and nonproliferative diabetic retinopathy.
FAQ’s for Macular Degeneration Vs Diabetic Retinopathy
Does diabetic retinopathy cause macular degeneration?
No, it does not, however, it can affect the macula and cause similar damage.
What is the difference between macular edema and diabetic retinopathy?
Macular edema can be a specific form of diabetic retinopathy when it affects the macula. Diabetic retinopathy can affect other parts of the retina though.
Is retinal and macular degeneration the same?
Macular degeneration is a form of retinal degeneration but in a specific location. Other forms of retinal degeneration occur in other locations and in different forms.
Does high blood sugar affect macular degeneration?
Diets high in fats and sugar are at much greater risk for AMD, so yes.
What is diabetic macular degeneration?
The correct term for this would be diabetic macular edema. This is when the tiny blood vessels of the macula are damaged by diabetes and they leak causing edema or swelling of the macula.
Is it true that diabetes causes fuzzy vision?
If your fuzzy vision is caused only by hyperglycemia or hypoglycemia, it should clear up with time and proper blood sugar management. Your blood sugar level — and, with it, your eyesight — may take several weeks to recover to normal. However, it’s possible that the impact is just transitory. If the fuzzy vision is from damage to the blood vessels and edema, the fuzzy vision could become permanent if not treated quickly.