When treating patients for diplopia, it’s crucial to ascertain whether their double vision is binocular or monocular. One method for doing so involves asking whether it disappears when covering one eye and whether certain directions (eg, vertical or horizontal) make matters worse.
Sudden diplopia requires prompt medical intervention; intermittent or fluctuating diplopia suggests an intermittent neurologic condition like myasthenia gravis or multiple sclerosis that requires additional medical investigation.
Causes
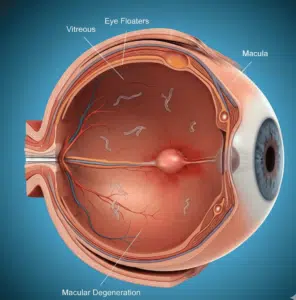
Diplopia is a common condition with numerous causes. Diabetes and hypertension, in particular, both of which restrict eye movement causing images to fall on different retinas. Other rarer causes may include compression of nerves in the head or eye socket area or malfunction of nerves due to loss of myelin sheath insulation and trauma – these cases require comprehensive examination by both an ophthalmologist and neurologist as soon as possible in order to diagnose and treat when necessary.
Diplopia should be diagnosed and classified according to whether it is monocular, binocular, and constant or intermittent, along with any associated pain that occurs with or without eye movement. Furthermore, noting if its intensity changes over time could indicate decompensated strabismus (esotropia/exotropia) or myasthenia gravis as these could indicate myopathy in those at risk of the disorder.
History is key in diagnosing patients. Timing of the onset should be noted as sudden onset usually requires immediate medical care. Other indicators may include history of vascular risk factors in older individuals that could indicate an intracranial mass lesion; Giant Cell Arteritis should be considered in younger individuals with variable diplopia.
At examination, an ophthalmologist will carefully observe both eyes for signs of proptosis or ptosis, examine pupil reactions to ensure equal and reactive pupils, perform motility testing with straight ahead, up/down diagonal and inward toward nose (“convergence”) tests, as well as whether diplopia occurs with or without eye movements.
As diplopia may be linked to other symptoms, such as headache or balance problems, it is crucial that we take note of any additional medical history or medications which could contribute to its cause, such as sedatives or analgesics that cause intracranial hypertension; corticosteroids or growth hormone may increase brain fluid pressure causing increased intracranial pressure; any such interactions must also be assessed through testing cerebrospinal fluid samples taken via lumbar puncture with cerebrospinal fluid testing if any suspected associations exist between issues and diplopia and its causes if any possible associations arises then further testing should take place through cerebrospinal fluid testing involving cerebrospinal fluid testing of cerebrospinal fluid testing can reveal any possible correlations if this exists between.
Diagnosis
An evaluation of patients with newly acquired diplopia begins by reviewing their history and taking vital signs (temperature, heart rate and blood pressure). Next comes an eye exam which involves noting initial position of eyes, measuring visual acuity both individually and jointly corrected and looking for signs of eye disease such as proptosis, ptosis, scleral depression deformities or dislocation such as corneal scarring and dislocation of lenses. Finally an ocular motility test is performed observing whether patients can follow an examiners finger across face from side to side, up and down diagonally towards nose (convergence).
Cover-uncover tests can also help assess whether deviation or strabismus is present with both eyes open (manifest/tropia) or only when one eye is covered (latent/tropia). Patients suffering from idiopathic intracranial hypertension often present negative visual field tests and normal motility exams but may exhibit narrowing of blood vessels of their retina as well as cotton wool spots or hard exudates on its surface indicating decreased blood flow to it during ophthalmoscopy examination.
Monocular diplopia is usually caused by intraocular pathology and more frequently seen among those diagnosed with eye conditions like cataracts or glaucoma than neurological causes. However, monocular diplopia may suddenly appear in patients suffering an ischemic stroke affecting Brodmann’s area 19 (frontal eye fields or cerebellar lesions), signaling possible vascular disease. Case 3 involved an individual who experienced episodic right monocular diplopia and headache. Neurological examination was unremarkable and an MRI brain revealed paroxysmal atrial fibrillation; furthermore, no other eye symptoms existed and her diplopia wasn’t linked with either her service-connected CVA or reported PTSD, and thus was denied entitlement to service connection for its causes.
Treatment
Diagnosing diplopia requires careful history-gathering and physical examination, including timing of its onset. Sudden or sudden-insidious diplopia should be assessed immediately; more gradual insidious onset diplopia requires evaluation but should still be addressed. It is also vitally important to determine whether the diplopia is consistent or intermittent; whether images overlap; whether any pain or eye movements accompany it; as well as its direction (upward, downward or horizontal), as well as whether its intensity level asymmetry or paretic or asymmetricality.
Treatment for diplopia will depend on its cause; for instance, diabetes or hypertension usually resolve on their own without intervention from medical personnel. Conversely, compression of nerves within the head and eye socket, or loss of their protective sheath must be closely evaluated by an ophthalmologist with frequent assessments such as quantitative visual fields to monitor response to treatment; should symptoms recur surgical procedures may include optic nerve sheath fenestration or shunting to treat these conditions.
Monocular diplopia should be evaluated in all patients presenting with headache and diplopia for signs of elevated intracranial pressure, including patients who also exhibit headache. A thorough ophthalmic and neuro-ophthalmic examination will help identify clinical features indicative of intracranial hypertension (IIH), allowing clinicians to conduct brain imaging with venography with normal results or, if not contraindicated, lumbar puncture; patients who have histories of hypertension, obesity or chronic meningitis should receive treatment via acetazolamide for treatment of IIH.
Prevention
Hypertension diplopia can often be prevented by maintaining a healthy weight so as to not increase body pressure too significantly, not smoking and taking prescribed dosages of any medications for your condition. Furthermore, visiting your physician regularly allows him or her to monitor your blood pressure and ensure you’re receiving appropriate dosages of any needed medicines.
As soon as you notice blurry vision, regardless of its relationship to hypertension, it is wise to get an eye exam immediately. An examination can detect potential problems like presbyopia or computer vision syndrome that require treatment with multifocal glasses or surgery; and headaches associated with blurred vision could indicate another medical issue that needs urgent treatment.