Glaucoma steals vision silently from millions of people throughout the world. One of the most important things to comprehend about glaucoma’s negative impacts is how it affects the optic nerve. In this article, we will examine every facet of the subject, from comprehending the structure of the optic nerve to detecting optic nerve damage, talking about neuroprotection techniques, and investigating how Low Vision Services and Devices can significantly enhance the quality of life for glaucoma patients.
What Is the Optic Nerve?
Let’s first understand the optic nerve before discussing how glaucoma affects the optic nerve.
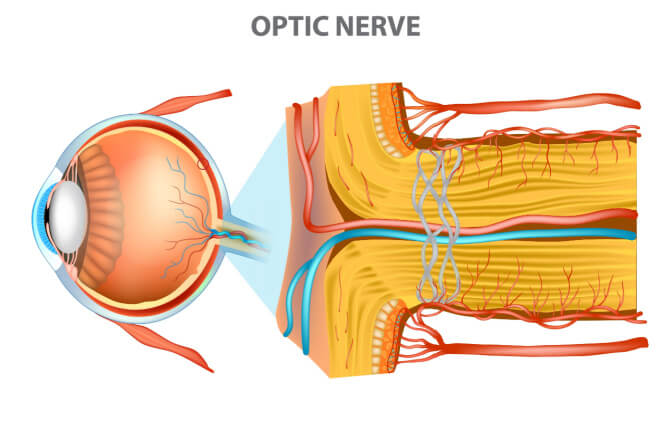
The body’s information superhighway for vision is analogous to the optic nerve. The link between the eye and the brain is made up of more than one million nerve fibers. The retina, the light-sensitive tissue at the back of the eye, sends visual signals through these fibers to the visual regions of the brain. Consider it as the cable that links your TV to your cable box; without it, no picture will be seen.
What Is the Optic Nerve Made Up Of?
Knowing the composition of the optic nerve is crucial to understanding how glaucoma affects it.
Nerve fibers, blood vessels, and connective tissue make up the optic nerve. Together, these elements make sure that visual information flows smoothly from the eye to the brain. Any harm to these components can obstruct this crucial channel, resulting in visual issues.
How Is Damage to the Optic Nerve Determined?
In order to properly manage glaucoma, early diagnosis of optic nerve damage is essential. But how do eye doctors find this damage?
The visual field test is one of the main diagnostic tools. Your doctor can locate any regions of vision loss by using this test to map out your peripheral vision. It is important to comprehend what the visual field test tells your doctor in order to follow the progression of glaucoma and make wise treatment choices.
What Does My Doctor Learn from the Visual Field Test?
How to Interpret the Visual Field Test:
The visual field test, sometimes referred to as perimetry, evaluates both your central and peripheral vision. It aids in locating any irregularities or areas of vision loss. This is how the test usually proceeds:
Patient Preparation: One eye will be covered as you sit in front of a bowl-shaped device. The second eye is fixed on the center of the scene.
Tiny lights will flash in various locations within your field of view as a light stimulus. Each time you notice a light flash, you must hit a button.
The instrument records your answers to the lights in a systematic manner throughout the test, mapping your visual field as it goes.
What Doctors Look for in the Results:
Your eye doctor will carefully examine the data and use their knowledge to interpret the visual field test results. They look for the following:
Finding any visual field defects is the most important part of the process. These are the regions where you were not able to see the light stimuli, indicating vision loss.
Patterns of Defects: To identify where and how severe a defect is, doctors look at its pattern. Defect locations can reveal important details about the portion of the optic nerve that is impacted by glaucoma.
Depth and Progression: When assessing the severity of glaucoma and the rate at which it is progressing, it is important to consider both the depth of defects (how black they appear on the test) and their progression over time.
The stages of glaucoma are determined by certain patterns:
The visual field test can identify distinct patterns of vision loss that aid in glaucoma stage determination. Among these patterns are:
Early Stage Glaucoma: Peripheral vision is frequently affected first in the early stages of glaucoma. In the visual field, isolated, minor abnormalities are sometimes found at the boundaries.
Glaucoma in the moderate stage causes broad visual field abnormalities that can sometimes spread into the central vision. Damage to the optic nerve may also manifest as cupping.
Glaucoma in its advanced stages can have severe visual field abnormalities, which could result in tunnel vision, where only a tiny core area is still visible. Cupping of the optic nerve becomes noticeable.
Glaucoma in its last stage causes severe vision loss and can shrink the visual field to a single, small island in the center. Cupping the optic nerve is significant.
It’s important to remember that visual field exams are frequently carried out, enabling your doctor to track changes over time. Making treatment options and halting additional vision loss can both be helped by spotting tiny changes in the visual field.
OCT’s Use in Glaucoma Detection
OCT is a cutting-edge diagnostic technique that has revolutionized the field of ophthalmology and is essential for the early diagnosis and treatment of glaucoma.
Recognizing OCT
Let’s quickly define OCT before getting into its involvement in the identification of glaucoma. OCT uses light waves to produce high-resolution cross-sectional images of the interior anatomy of the eye in a non-invasive manner. The retina, the head of the optic nerve, and other significant ocular components may all be seen in fine detail and in real-time.
glaucoma, the optic nerve, and
As was previously mentioned, the optic nerve is the main organ affected by glaucoma. Vision loss can result from optic nerve fiber injury brought on by elevated intraocular pressure (IOP). For effective care and limiting any harm, early diagnosis of these alterations is essential.
How does OCT operate?
OCT operates on the interferometry tenet. It does this by projecting a beam of light into the eye, which is then returned. OCT produces precise images of the internal structures of the eye, including the optic nerve head and the retinal nerve fiber layer (RNFL), by timing the time it takes for the light to return and examining its interference patterns.
OCT’s Function in Glaucoma Detection
Measurement of RNFL Thickness: The thinning of the retinal nerve fiber layer is one of the main signs of glaucoma. OCT enables ophthalmologists to precisely assess RNFL thickness, supplying important knowledge regarding the health of the optic nerve fibers. The RNFL can thin early in the course of glaucoma, frequently before any obvious visual abnormalities become apparent.
How to Spot Changes in the Optic Nerve Head:
Glaucoma can also cause structural alterations in the optic nerve head, such as cupping. OCT enables accurate cup-to-disc ratio measurements by providing comprehensive pictures of the optic nerve head. Increased cup-to-disc ratio is a glaucoma warning sign and a marker of optic nerve damage.
- Monitoring Progression: OCT is useful for both glaucoma diagnosis and monitoring the disease’s development over time. Doctors are able to modify treatment strategies as necessary by comparing serial OCT scans to spot small changes in RNFL thickness or optic nerve head characteristics.
- Evaluation of Treatment Effectiveness: Ongoing care is crucial for glaucoma sufferers. By observing changes in the optic nerve and RNFL, OCT assists in evaluating the efficacy of treatment. These scans may reveal stable or enhanced parameters after a successful treatment.
- Making a Difference Between Glaucoma and Other Eye Conditions: OCT can assist in making a difference between glaucoma and other eye conditions that may have comparable symptoms. This distinction is essential because, depending on the underlying illness, the treatment strategy can differ greatly.
Benefits of OCT for Detecting Glaucoma
- Non-invasive: OCT is a non-invasive process; no needles or incisions are needed. A little discomfort is felt by the patient during the scan.
- Great Precision: OCT offers cross-sectional pictures of great resolution, enabling accurate assessments of key ocular structures.
- Early Detection: OCT can spot glaucoma early on, frequently before any visible visual problems appear. In people with glaucoma, maintaining vision depends on early identification.
OCT offers objective measurements, which lessens the subjectivity inherent in some other diagnostic methods.
The way we diagnose and treat glaucoma has been changed by optical coherence tomography (OCT). It provides for early identification, precise diagnosis, and efficient glaucoma progression monitoring due to its capacity to produce detailed, real-time images of the optic nerve head and retinal nerve fiber layer. OCT, a non-invasive and extremely accurate instrument, has emerged as a crucial ally in the battle against this blinding condition, providing glaucoma patients with hope and better outcomes.
What Causes Optic Nerve Degeneration?
Better treatment and prevention of glaucoma depend on knowing the underlying causes of optic nerve degeneration.
The most common cause of glaucoma is elevated intraocular pressure (IOP), which over time can harm the optic nerve. We’ll look into how genetics, IOP, and other risk factors contribute to the onset of glaucoma.
Genetics:
- Family history: Glaucoma is strongly predisposed genetically. A higher chance of acquiring glaucoma exists in people with a family history of the disease. Different kinds of glaucoma, such as primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG), have been linked to a number of genes.
- Gene mutations: Certain genetic changes can make people more vulnerable to glaucoma. Genes including MYOC, OPTN, and CYP1B1 have been related to glaucoma in various ways.
IOP, or intraocular pressure:
- Elevated IOP: Glaucoma is widely known to develop and progress as a result of elevated intraocular pressure. Increased IOP has the potential to harm the retinal ganglion cells and optic nerve, which transport visual information to the brain.
- Mechanism: Aqueous humor, the fluid that fills the eye, may produce more or drain more slowly in cases of high IOP. The optic nerve head may experience mechanical stress due to an imbalance between production and drainage, which may eventually cause injury.
Other danger elements
- Age: People over 60 are at higher risk for glaucoma, whose risk rises with age.
- Race and Ethnicity: Some racial and ethnic groups, like African Americans and Hispanics, are more likely to develop glaucoma and may also be more likely to have a more severe version of the condition.
- Eye Anatomy: Glaucoma risk may be influenced by the anatomical makeup of the eye. For instance, angle-closure glaucoma risk can be increased by a shallow anterior chamber angle.
- Medical conditions: Glaucoma risk can be raised by some medical diseases, including diabetes and hypertension.
- Eye Trauma: Eye trauma increases the risk of glaucoma and damages the optic nerve.
- Use of Steroids: Long-term use of corticosteroid drugs, whether taken orally or as eye drops, can raise IOP and raise the chance of developing glaucoma.
Protecting the Optic Nerve (Neuroprotection)
The goal of neuroprotection strategies is to maintain and safeguard the health and functionality of nerve cells (neurons) in the central nervous system, which includes the brain and spinal cord. These methods are frequently used in the context of neurological illnesses such as brain traumas, neurodegenerative diseases, and other neurological conditions. Here are a few methods for neuroprotection:
Antioxidant Therapy:
Neurons can be damaged by oxidative stress, which is brought on by the accumulation of dangerous chemicals called free radicals. Vitamins C and E, selenium, and antioxidants like coenzyme Q10 can all assist in lowering oxidative stress and protect neurons from injury.
Neurotrophic elements
Proteins known as neurotrophic factors aid in the development, maintenance, and proliferation of neurons. Examples include nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF). These elements can be treated with drugs or encouraged by engaging in physical activity and mental stimulation.
Inflammation prevention techniques
Many neurological diseases are linked to chronic inflammation. Neurons can be protected by reducing inflammation using drugs, dietary changes (anti-inflammatory diets), and lifestyle adjustments.
Intermittent fasting and calorie restriction:
Intermittent fasting and calorie restriction have both demonstrated potential advantages for neuroprotection. They might boost brain health, improve cellular repair procedures, and lessen oxidative stress.
Exercise:
Regular exercise is linked to enhanced neuroprotection and brain health. Exercise improves brain function overall by increasing blood flow to the area and stimulating the production of neurotrophic substances.
Mental Exercise:
Playing mental games, reading, picking up new skills, and socializing can all assist in retaining cognitive function and ward off neurodegenerative conditions like Alzheimer’s disease.
Neuroprotective Drugs:
Specific neurological diseases are treated using medicines that have neuroprotective qualities. Disease-modifying medications, for instance, can stop the progression of multiple sclerosis (MS) and safeguard nerve fibers.
Lifestyle changes:
Supplements with vitamins and minerals:
Optic nerve health can be aided by leading a healthy lifestyle.
A balanced diet and regular exercise can help manage diseases like diabetes and hypertension, which can make glaucoma worse.
Avoid consuming too much caffeine as it may momentarily increase IOP.
Numerous nutrients, including vitamin D, B vitamins (including folate and B12), and omega-3 fatty acids, may have neuroprotective properties.
Given the significance of the optic nerve, safeguarding it is crucial, especially for those who have glaucoma.
Medications and Eye Drops:
In glaucoma, maintaining proper intraocular pressure (IOP) control is essential for protecting the optic nerve.
Your eye doctor’s prescription eye drops or medications may help lower an elevated IOP.
It is important to follow the recommended treatment plan in order to keep IOP levels steady and avoid optic nerve damage.
Treatment Compliance:
- Follow your doctor’s advice and recommended course of action religiously.
- Keep up with routine checkups to monitor IOP and modify your treatment as appropriate.
- Openly discuss any worries or drug side effects with your doctor.
Protect Your Eyes:
- When engaged in activities that could cause eye injury, wear protective eyewear.
- To protect your eyes from damaging UV rays, put on UV-protective sunglasses.
- Injury to the eye, which could exacerbate glaucoma, can be avoided with adequate protection.
Stress management
Chronic stress may have an impact on IOP. To relieve tension, try relaxing activities like yoga or meditation.
Make sure you receive enough sleep to improve your eye health generally and lower your stress levels.
Nutritional Supplements:
According to certain research, antioxidant vitamins (such as vitamins C and E) and other dietary supplements may have a neuroprotective effect on the optic nerve.
Before including supplements in your regimen, talk with your eye doctor about their use.
Quitting Smoking:
The optic nerve is known to suffer damage from smoking.
In addition to enhancing general health, quitting smoking can lower the chance of optic nerve injury.
Keeping an eye on your general health:
It’s possible that conditions like migraine and sleep apnea will affect optic nerve health.
Regularly evaluate your general health, and take immediate action to address any medical concerns.
Preventing Ocular Hypertension:
Ocular hypertension, or elevated IOP without obvious glaucoma damage, may put a person at risk for glaucoma.
To avoid optic nerve injury, ocular hypertension must be regularly monitored and perhaps treated.
Experimental Therapies
Educate yourself on new glaucoma neuroprotective treatments.
Future clinical trials and research could lead to the development of novel therapies to protect the optic nerve.
Devices and Services for Low Vision: Improving Quality of Life
Although managing glaucoma can be difficult, improvements in low vision services and equipment have given those who are affected new options. These products and services can considerably enhance the quality of life for glaucoma sufferers.
The Diverse Low Vision Services Approach
The special requirements of those with limited vision are addressed holistically by low vision services. These services cover a variety of tactics and tools aimed at maximizing the remaining vision and encouraging independence. For those who have reduced vision due to glaucoma, low vision services can be helpful.
Complete Vision Evaluation
Low vision specialists carry out extensive evaluations to ascertain the degree of visual impairment, the particular difficulties the person is facing, and their objectives. A customized plan is built on the results of this examination.
Choosing Assistive Technology
Prescriptions for assistive devices made specifically for glaucoma patients are one of the main ways low vision services benefit those with the condition. Magnifiers, telescopes, electronic magnification systems, and screen-reading software are a few examples of these tools. These technologies make it easier for people to read, write, and carry out daily duties.
Vision Rehabilitation
The provision of low vision services must include vision rehabilitation. It entails educating glaucoma patients on how to make the most of their remaining eyesight. They use methods like eccentric seeing (using their peripheral vision), boosting contrast, and enhancing the lighting in their homes.
Adaptive Techniques
Low vision specialists collaborate with clients to create daily-life adaptations. They might be instructed on how to designate appliance controls for ease of use, organize their houses for safety, and confidently navigate their surroundings by using tactile clues.
Training in Orientation and Mobility
Training in mobility and orientation is crucial for people with severe vision loss. They gain the knowledge and abilities necessary to move around alone, use public transportation, and preserve their independence.
Psychological Support
Losing one’s vision can be emotionally difficult to deal with. In order to help people deal with the emotional and psychological effects of their disease, low vision programs frequently incorporate psychological counseling. Counseling and support groups may be helpful in this regard.
Access to Community Resources
The providers of low vision services have strong ties to neighborhood resources. They can aid people in getting access to services including support groups, transportation assistance, and specialized educational programs.
Low Vision Equipment and Aids
Low vision services may offer low vision aids and equipment, such as customized eyeglasses, filters, and tinted lenses, to improve vision and lessen glare in addition to assistive electronic devices.
Training and Education
Specialists in low vision provide information to patients and their families on glaucoma, its progression, and practical management techniques. People are more equipped to actively contribute to their eye health with this knowledge.
Regular Monitoring and Modification
Services for people with low eyesight are not static; they change as the needs of the person change. Regular follow-up evaluations are performed by specialists to make the required modifications to the treatment plan and assistive technology.
FAQs
What impact does glaucoma have on peripheral vision and the optic nerve?
The optic nerve is largely hurt by glaucoma, which can cause a gradual loss of peripheral vision. Early diagnosis and therapy are essential to halt future eyesight loss.
Does glaucoma lead to thinning of the optic nerve?
Yes, optic nerve atrophy—a thinning of the optic nerve—is frequently caused by glaucoma. As the nerve fibers sustain increasing damage, this happens.
How soon does glaucoma cause damage to the optic nerve?
Individuals with glaucoma have optic nerve degeneration throughout different time periods. While some may advance quickly, others may progress more slowly. Examining and monitoring your eyes regularly might help you detect changes.
What are the phases of optic nerve glaucoma?
Depending on how much the optic nerve has been damaged and how much vision has been lost, glaucoma stages can be divided into early, intermediate, and advanced stages. There could be several treatment modalities needed for each stage.
Conclusion
We have covered every aspect of how glaucoma affects the optic nerve in this extensive article, from its structure and detection to the reasons for degeneration and neuroprotection techniques. We’ve also emphasized how poor vision services and equipment can significantly improve the quality of life for glaucoma sufferers.
Remember that the best way to combat this sight-stealing disorder is through information and proactive management. You can take charge of your eye health and protect your priceless eyesight by comprehending the subtleties of how glaucoma affects the optic nerve and making use of the resources at your disposal.