What is Degenerative Myopia?
Up to 3% of people worldwide suffer from a subset of myopia known as pathologic myopia. Pathologic myopia-related vision loss has significant medical consequences because it can be gradual, permanent, and afflict people in their prime working years. High myopia is characterized as having at least a -6.00D refractive error or an axial length of at least 26.5mm. Early studies’ definitions of pathologic myopia varied and frequently focused on the interaction between refractive error and axial length, which may only signify a severe case of myopia. Additionally, the proposed cutoff values were not supported by any convincing evidence. The definition of pathologic myopia has changed in recent years to read “the presence of myopic maculopathy equal to or more severe than diffuse chorioretinal atrophy.” Diffuse, patchy, lacquer cracks, myopic choroidal neovascularization (myopia CNV), and CNV-related macular atrophy are all symptoms of myopic maculopathy.
Causes of Degenerative myopia?
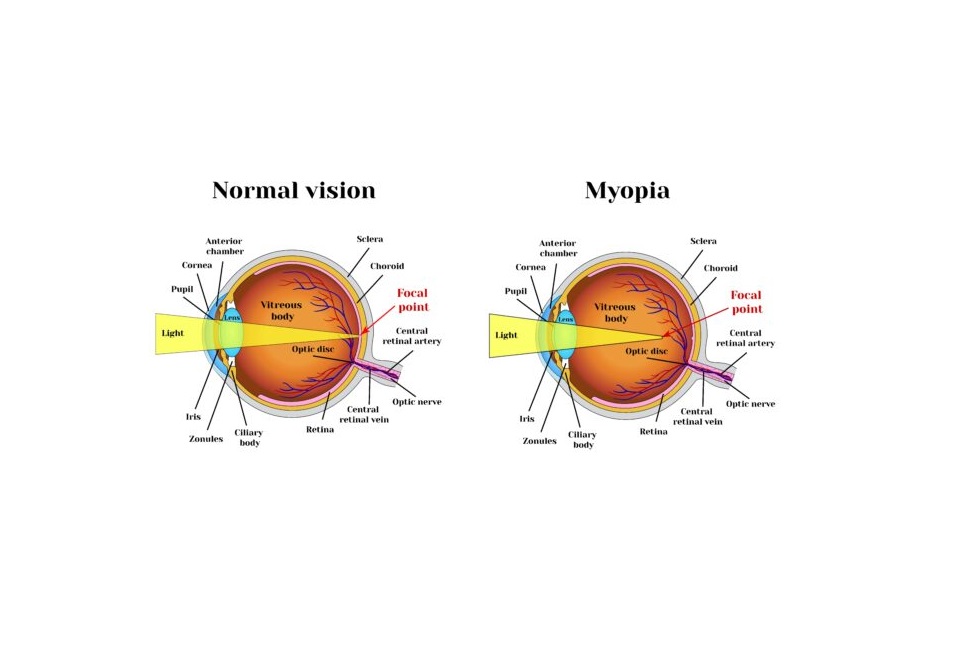
In myopia, light rays are focused in front of the retina. As a result, close things can be seen clearly while distant ones appear hazy. However, reading close to the face may become difficult if near vision deteriorates more.
One of the following three conditions can cause myopia:
- The cornea (the eye’s front surface) is too powerful because it is too curved.
- The eye is too long, from front to back, or a combination of both.
- Myopia often stabilizes once the growth phase is over, at which point corrective lenses can return vision to normal. On the other hand, increased myopia is frequently hereditary, which means that if one parent is moderately or severely nearsighted, the likelihood that one of the children will be myopic is higher.
A form of myopia known as juvenile-onset begins in childhood and almost always gets worse as you age.
Myopia that is severe, such as degenerative myopia, increases the chance of blindness and vision loss.
The distortion of the eye causes stress on the retina, which is vulnerable to injury or detachment and can significantly impair visual acuity.
Degenerative Myopia Symptoms
The following are some of the most typical degenerative myopia signs and symptoms:
- The gray area in the field of vision
- Straight lines look warped.
- Color perception changes
- A decrease in contrast sensitivity
- Central vision loss
- Reading issues
- Difficulty identifying faces
Pathophysiology
A kind of myopia (nearsightedness) called degenerative myopia, often referred to as pathological or high myopia, is connected to a number of ocular issues and may result in permanent vision loss. Degenerative myopia has a complicated pathophysiology that involves alterations in the structure and operation of numerous ocular tissues.
The extreme elongation of the eyeball, which causes the retina to be stretched and thinned, is one of the key alterations in degenerative myopia. Retinal atrophy and degeneration may result from this, which can impair vision. The abnormal axial elongation that results from a confluence of hereditary and environmental factors is assumed to be the outcome of an imbalance in the usual processes of ocular growth and development.
The sclera, the eye’s white outer covering, and the choroid, a layer of blood vessels that nourishes the retina, both experience further changes in degenerative myopia. In degenerative myopia, the sclera may weaken and become thinner than usual, making it more prone to stretching and distortion. Retinal atrophy may also develop as a result of the choroid being thinner and less capable of supplying the retina with sufficient blood flow.
Degenerative myopia is linked to functional changes in the retina, such as decreased light sensitivity and visual understanding, in addition to these structural alterations. The stretching and thinning of the retina as well as anomalies in the brain’s processing of visual information are thought to be the causes of these functional alterations.
Degenerative myopia has a complicated and multifaceted etiology that affects many aspects of the eye’s structure and function. Degenerative myopia’s underlying mechanisms are not fully known, but research into this ailment has resulted in the creation of novel therapies that try to protect the eyesight of those who suffer from it.
Risk Factors
The onset of degenerative myopia is accompanied by various risk factors. The following are some of the most well-known risk factors:
Genetics
Genetics is recognized to play a significant role in degenerative myopia. Degenerative myopia is more likely to affect people with a family history of the disorder.
Age
Degenerative myopia usually starts in childhood or adolescence and tends to get worse with time. The risk of complications related to degenerative myopia is increased in people over the age of 40.
Ethnicity
According to studies, people of Asian ancestry have a higher risk of developing degenerative myopia than people of European ancestry.
Environment
A higher risk of acquiring degenerative myopia has been linked to a number of environmental factors. These include exposure to strong light, insufficient outside time, and long stretches of near work (such as reading or using a computer).
Gender
According to certain research, women may be slightly more likely than men to suffer degenerative myopia.
Refractive error
Degenerative myopia is more likely to develop in people with higher levels of myopia (nearsightedness).
Other medical conditions
Degenerative myopia has been linked to an increased risk of developing several ailments, including diabetes and connective tissue diseases.
It is crucial to remember that while having one or more of these risk factors may raise an individual’s risk, it does not guarantee that they will develop degenerative myopia. For the prompt diagnosis and treatment of degenerative myopia, routine eye exams and the early detection of myopia are crucial.
Degenerative Myopia Treatment
The vision loss caused by degenerative myopia is frequently irreversible.
Your eye doctor will weigh several therapy choices to aid patients’ vision quality while restoring their eyesight, including:
- Glasses: Thick-lens prescription glasses can aid in the improvement of a person’s vision.
- Contact lenses: Some individuals may be able to replace their glasses with prescription contacts to enhance their vision.
- Intraocular lenses: IOLs are synthetic lenses that can be used in place of the natural lenses in the eyes. Some people with degenerative myopia have reported that this is helpful.
- Anti-VEGF therapy entails taking drugs that prevent macular degeneration-causing new blood vessels from growing in the retina.
- Treatment for aberrant blood vessels in the retina that may be causing vision loss utilizing photodynamic treatment (PDT).
- In order to help with the repair of retinal tears or detachments, a technique known as a vitrectomy involves partially or completely removing the vitreous gel from inside the eye.
Physical Evaluation
It is crucial to evaluate visual acuity, intraocular pressure, pupillary response, and a dilated fundus exam. Finding issues associated with pathologic myopia requires a careful macular examination and a peripheral depression assessment. Lacquer cracks (LC), retinal schisis, or choroidal neovascularization in the macular region, as well as holes or tears in the retina’s periphery. Amsler grid testing and visual field evaluation may be helpful.
Signs of Degenerative Myopia
Throughout the fundus, there is progressive thinning and attenuation of the retinal pigment epithelium (RPE). Even in young patients with high myopia, a tessellated appearance due to a dispersed pattern of RPE atrophy and fluctuating light reflection may be noticed. This hypopigmented appearance is known as peri-papillary atrophy when RPE attenuation surrounds the optic disc.
The optic disc is frequently referred to as a tilted disc and has an oval shape on the front. It seems as though the optic nerve enters the expanded globe at an angle. The disc’s temporal flattening, which results from peri-papillary scleral expansion in part, gives the appearance of being tilted. Where the sclera is clearly visible, a hypo-pigmented myopic crescent is seen. Under the atrophic RPE, choroidal arteries will be more noticeable in intermediate diseases. However, as the condition progresses, the choroid itself atrophies, and the choroidal veins may lose some of their prominence.
In 4.2% of eyes with an axial length of at least 26.5mm, lacquer cracks—irregular, yellow-looking bands—are visible in the posterior pole. These are Bruch’s membrane cracks and might develop into choroidal neovascularization (CNV) foci later on. According to reports, 29.4% of individuals with lacquer cracks go on to develop CNV. These breaks may eventually resemble geographic atrophy, comparable to advanced non-neovascular Age-related Macular Degeneration (AMD), as they can grow and extend over time.
Fuchs spots, also known as Forster-Fuchs spots, are regions of RPE hyperplasia that are thought to be the RPE’s reaction to previously regressed CNV. In 5% to 10% of cases of degenerative myopia, myopic CNV has been described as the most frequent cause of visual loss in high myopia.
A common occurrence, believed to occur in 35% of eyes with high myopia, is staphyloma formation, which is defined by the outpouching of scleral tissue generally involving the optic disc or macula. With biomicroscopy, this may be challenging to see, but it is clear on OCT or B scan ophthalmologic ultrasonography. Lacquer cracks, RPE attenuation, epiretinal membrane, and macular or foveal schisis are frequently linked to staphylomata.
Types and Classifications of Myopia
Based on the severity of the disorder and any accompanying problems, degenerative myopia is divided into a number of categories. For the diagnosis, prognosis, and therapy of the illness, these classifications are crucial. Here are a few of the most popular categories:
Refractive myopia
Refractive myopia is the most prevalent type of myopia and causes blurry distance vision due to the elongation of the eyeball.
Pathological myopia
This type of myopia is more severe and is characterized by structural changes to the eye, such as thinning of the retina and choroid as well as straining and thinning of the sclera. Pathological myopia can cause a number of issues, including macular atrophy, choroidal neovascularization, and retinal detachment.
High myopia
Another name for myopia with a significant amount of refractive error, usually greater than -6.00 diopters. High myopia is frequently linked to ocular pathology changes and a higher risk of problems.
Posterior staphyloma myopia
Myopia with a posterior staphyloma is referred to as posterior staphyloma myopia. Posterior staphyloma is a bulge at the back of the eye caused by stretching and sclera thinning. A higher risk of problems such as retinal detachment is linked to posterior staphyloma myopia.
Retinal detachment and macular holes are two consequences of degenerative myopia that might lead to surgery. Degenerative residual myopia is the residual myopia that is left over after surgery.
An international team of high myopia specialists created a simpler, systematic categorization using a meta-analysis of (META-PM) pathologic myopia in response to the lack of a standardized diagnosis and vocabulary for pathologic myopia. Based on atrophic alteration, myopic maculopathy was divided into five separate groups.
- No macular degenerative lesions fall into category 0.
- tessellated fundus alone in category 1
- Diffuse chorioretinal atrophy, category 2.
- Patchy chorioretinal atrophy, category 3.
- Macular atrophy, category 4.
An atrophy-centered classification approach is not adequately representing many patients with macular alterations brought on by pathologic myopia, as has recently been recognized. ATN (atrophic, tractional, and neovascular) is a recently proposed classification system for myopic maculopathy.
Overall, structural changes in the eye, related problems, and myopia severity are used to categorize degenerative myopia. Depending on the situation and goal of the diagnostic, a different classification may be employed.
Summary
Degenerative myopia, sometimes referred to as pathological or high myopia, is a disorder marked by excessive eyeball elongation that causes severe myopia and its repercussions. The retina, choroid, and sclera are only a few of the ocular structures whose structure and function are altered by degenerative myopia. Genetics, age, ethnicity, environment, refractive error, and specific medical disorders are all risk factors for degenerative myopia. Based on the severity of the disorder and any accompanying problems, degenerative myopia is divided into a number of categories. For the diagnosis and treatment of degenerative myopia, routine eye exams and early myopia detection are crucial. Depending on the particular difficulties and severity of the condition, other treatment options, such as corrective lenses, medication, and surgery, may be available.
FAQ’s
What distinguishes myopia from degenerative myopia?
Although many people are aware of what myopia (nearsightedness) is, there is a specific type of myopia that worsens over time, making it considerably more challenging to see both near and far objects and that is degenerative myopia.
How can you tell if myopia is a degenerative condition?
The signs of degenerative myopia: Faces are difficult to recognize. changes in how we perceive color. a dark area in the field of vision. a poor sense of contrast.
Is degenerative myopia considered a disability?
Nearsightedness, or myopia, is not typically regarded as a handicap in the United States. It does not qualify a person for government assistance or ADA modifications. However, if untreated, excessive myopia that progresses can cause blindness and vision loss these can be considered disabilities.