Angle recession glaucoma is a disease that happens when the eye suffers from blunt force trauma. If you get hurt, the drainage part of the eye is damaged and can cause the fluid inside the eye to back up.
This can lead to inflammation and degenerative changes, which block the pathway that your eye’s fluids use to drain. High intraocular pressure (pressure inside the eye) can be caused by too much fluid buildup, which can then lead to angle recession glaucoma.
Angle recession glaucoma doesn’t happen to everyone who has been through stress, but it may happen faster in people who are genetically more likely to get it.
If you don’t get diagnosed with glaucoma or take care of it properly, you could go blind permanently. Also, anyone who has had an eye injury should see an eye doctor every year.
Mechanism of Action
As a result of direct or non-penetrating injuries to the eye, the angle recedes. In this kind of injury, the force goes from the front to the back of the eye, expanding along the equator. Structures along the equator, like the ciliary body, are most likely to be damaged.
There are both long and short fibers in the ciliary body, and they work against each other. The outermost longitudinal fibers contract from front to back, and the interior circular fibers contract from top to bottom. The part that is most likely to get hurt is the oblique middle zone, which is less well-known and not as strong. The oblique fibers can get torn when there is rapid axial expansion. When there is a quick change in the shape of the globe, aqueous fluid is also thrown toward the ciliary body, which could make the injury worse.
It’s good to know what the structures are to better understand how blunt injuries can cause high eye pressure and glaucoma. What is the angle of the eye? It’s where the pupil (the white part of the eye) meets the colored ring-shaped muscle called the ciliary body. The trabecular meshwork is a ring-shaped structure that looks like a sieve and is inside the angle. It links to the canal of Schlemm, which is also a ring-shaped chamber.
A structure called the ciliary body normally makes a clear liquid (aqueous humor) all the time inside the eye. The aqueous fluid moves around inside the eye and then flows into the veins. On its way out, it goes through the trabecular meshwork and the canal of Schlemm.
This steady flow of fluid is important because it brings nutrients to the inner eye and removes waste. But if something stops the watery fluid from leaving the eye, pressure builds up inside it.
Should you get hit in the eye hard, the iris can tear where it connects to the sclera (iridodialysis of the iris root), the ciliary body can tear (cyclodialysis), and/or the trabecular meshwork can get hurt.
There are two ways that the outflow of fluid is changed. First, the presence of blood and inflammatory cells that plug the trabecular meshwork may cause an instant rise in intraocular pressure. Second, the injury to the eye can change the shape of the trabecular meshwork in a way that can’t be undone. This makes it harder for fluid to pass through. This leads to high eye pressure that lasts for a long time. In some cases, it’s not noticeable, but if it’s not addressed, it can damage the optic nerve and cause glaucoma.
Demographics it affects
Angle recession glaucoma can start soon after an eye injury that doesn’t go all the way through or it can show up 50 years after the injury. Most of the time, the patient has forgotten all about the problem by the time they go to the eye clinic to worry about losing their sight. When this happens, the ophthalmologist helps the person remember any eye injuries they may have had to figure out why they are losing their sight.
Glaucoma doesn’t happen to all eyes with angle recession. It might or might not cause glaucoma, and the patient stays steady even after the gap recedes. But all of these cases need to be checked on regularly to make sure nothing bad happens.
Eye damage is always a part of angle recession, which can lead to glaucoma. There are, however, a lot of things that can go wrong with the eyes that can cause angle regression.
Epidemiology
The total risk of eye trauma is thought to be 19.8%, and the 5-year risk is 1.6%. Every year, about 2.4 million eye accidents happen in the United States. One study found that people who have had a closed-globe trauma have a 19% chance of getting glaucoma. This is about six times higher than the chance of getting glaucoma after a piercing injury. People who get a deep injury will go to the hospital right away, but people who get a blunt injury may or may not go to the hospital at all. So, the second group might not have been properly told about their damage and the possible outcomes.
Five to twenty percent of people who have severe angle recession will develop glaucomatous visual neuropathy. It’s possible that a higher risk of getting glaucoma can be predicted by an angle that recedes 180o or more. It’s interesting that up to half of the people whose angle recession gets worse and turns into glaucomatous optic neuropathy will also get glaucoma in the eye that wasn’t hurt. This finding shows that some people are more likely to get the disease and that the trauma sets off a chain of events that leads to glaucomatous optic neuropathy.
Signs and symptoms
At first, you might not have any signs. When you have glaucoma, high eye pressure hurts the nerve cells in your eyes over time. Over time, your vision can get worse in some places. But you might not notice them until most of the nerve fibers in your eyes have died.
Most of the time, you lose your side vision first. You lose sight in that eye if all the fibers in your optic nerve die.
It works the same way for people with angle recession glaucoma. If you get hurt, it could be years before you notice any changes in your vision. By the time cataracts set in, some people may even forget they were hurt.
After your eye heals from the injury, you’ll need to see an eye doctor who knows what to look out for once a year. They will check for angle decline and look for any signs of glaucoma in the eye.
Finding the cause
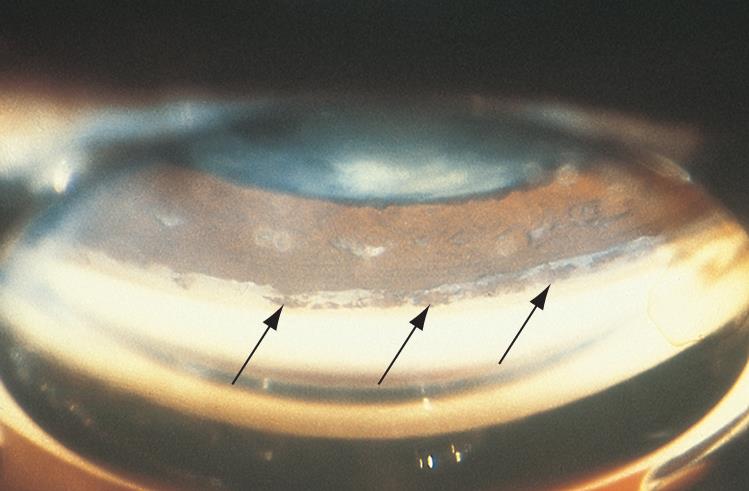
The eye doctor will look at your eyes and vision and ask you about your health history. As part of any medical eye test, they will check your eye pressure. A gonioscopy is the test they will use to look at the flow angle of your eye. The doctor will numb your eye with drops and then put a special lens on it. Then, a stream of light will be used to check the drainage angle for any damage or blockages that might cause the eye pressure to rise.
A “visual field” test will also be done to look for vision loss in the edges of your field of vision that you might not even be aware of. Your doctor may also check for damage to your optic nerve and measure the pressure inside your eye with other tests.
Your doctor may send you to a glaucoma specialist who treats glaucoma if the condition is very bad.
Treatment
Choices for Treatment Drugs. In an urgent setting, the goal of treatment should be to lower IOP and keep inflammation under control. Topical steroids and cycloplegic drugs are used to ease pain and inflammation. As first-line IOP-lowering drugs, aqueous suppressants are recommended. In theory, prostaglandin analogs can help by raising uveoscleral drainage, which gets around the problem with the trabecular meshwork. You should stay away from miotics because they can make your IOP go up for no reason, probably because they slow down the flow of fluid out of your eyes.
Use a laser. Laser trabeculoplasty doesn’t work for angle-recession glaucoma because it changes the shape of the angle and leaves scars on the trabecular meshwork. A different laser technique called Nd: YAG laser trabeculopuncture has had varying levels of success. It worked better when some of the trabecular meshwork structure was still visible on gonioscopy, which let the laser go deeper into Schlemm’s canal and improve the flow of urine.
Operating room. In angle-recession glaucoma, filtration treatment is less likely to work than in primary open-angle glaucoma. Using antimetabolites along with trabeculectomy can help it work better. When antimetabolites were used with trabeculectomy, researchers found that IOP dropped more than when trabeculectomy or Molteno tube insertion was used alone.
Some glaucoma drainage devices have been shown to help, but they don’t work as well for angle-recession glaucoma as they do for other types. For eyes that can’t see well, a cyclodestructive treatment might be a choice.
Conclusion
Angle recession can lead to long-term vision loss if not properly monitored and treated. It can, however, have the risk associated with getting it minimized by safety precautions when doing certain activities. Since almost all angle recession is caused by blunt trauma to the eye, taking extra safety measures when doing things like playing sports, playing paint ball, boxing, etc can greatly minimize ever having to deal with it in the first place. So wear your safety glasses, be aware of your surroundings, and wear helmets and headgear for dangerous activities.
FAQ’s
How can you keep from getting narrow-angle glaucoma?
Things You Can Do to Avoid Narrow Angle Glaucoma
Laser Peripheral Iridotomy (LPI) is usually the first treatment used for people who already have narrow-angle glaucoma or whose eye doctor thinks they are more likely to get it. Lasers are used to make a small hole in the edge of the eye. This makes the angle bigger and lets more fluid run through.
Can angle recession glaucoma be cured?
People who have had damage to their eyes can get this type of glaucoma. It can’t be fixed, but if you catch it early enough, you can get treatments to keep it from taking away your sight.
Are people with narrow angles more likely to get glaucoma?
If your angles aren’t very wide, does that mean you have glaucoma? Acute angle closure glaucoma and chronic angle closure glaucoma are both possible in people whose “angle” is small. But it’s important to know the difference between having glaucoma and being at risk for it.
What’s the difference between iridodialysis and angle recession?
When the circular and linear fibers of the ciliary body tear, this is called angle recession. When the ciliary body comes loose from where it attaches to the scleral spur, this is called cyclodialysis. When you do iridodialysis, you separate the iris root from where it connects to the anterior ciliary body.
What is the best way to treat glaucoma with angle recession?
Topical steroids and cycloplegic drugs are used to ease pain and inflammation. As first-line IOP-lowering drugs, aqueous suppressants are recommended. In theory, prostaglandin analogs can help by raising uveoscleral drainage, which gets around the problem with the trabecular meshwork.