After years of helping patients navigate vision loss, one sentiment comes up again and again: “I feel helpless.”
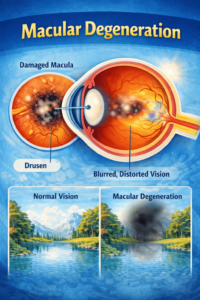
If you’ve been diagnosed with macular degeneration (AMD), I understand that fear. Vision loss feels incredibly personal, but I want to share some important news: You are not helpless.
Think of your treatment as a partnership. While your doctor provides medical care, you provide the daily self-care. By combining healthy lifestyle choices with professional treatment, you give your eyes the best possible chance of preserving your sight.
In 2019, an estimated 19.83 million Americans were living with AMD (modeled estimate; CDC/VEHSS, based on 2019 population). This guide will walk you through practical, manageable habits that help you take back control.
Understanding Your Role in Self-Care
Self-care is a vital part of your treatment plan. While you can’t change your genetics, you have power over your daily choices. By managing your diet, blood pressure, and habits, you give your eyes the best possible chance.
For dry AMD, focus on:
- AREDS2 Supplements: If recommended, these specific vitamins can slow the disease.
- Nutrition and Exercise: Fueling your body helps protect your sight.
- Monitoring: Use tools like the Amsler grid to catch changes early.
- Low Vision Aids: Use specialized lighting or magnifiers to stay independent.
For wet AMD, medical intervention is the priority:
- Stay Consistent: Never miss an injection or follow-up appointment.
- Watch for Sudden Changes: Report new wavy lines or dark spots immediately.
The sooner you build these habits, the better you can stack the odds in favor of your long-term vision. Taking proactive steps today helps preserve the sight you have for tomorrow.
Diet & Nutrition
Protect your macula with a nutrient-rich diet. Key nutrients like lutein, zeaxanthin, vitamin C, vitamin E, and zinc support eye health and slow vision loss. Add leafy greens, colorful veggies, citrus fruits, nuts, and omega-3-rich fish to your meals for stronger, healthier eyes.
- The Power of AREDS2 Supplements
If you have intermediate or advanced dry AMD, your eye doctor has likely mentioned “AREDS2” supplements. These aren’t just standard multivitamins. They are a specific formula known informally as macular degeneration self care vitamins proven to slow the progression of the disease in certain patients. Other powerful antioxidants such as NAD+, Liposomal Glutathione or GLY-NAC have shown amazing anti aging results.
What AMD Vitamins Can Do:
- Slow the progression of dry macular degeneration
- Support long-term eye health
- Help protect against oxidative stress with proper macular degeneration self care vitamins
What AMD Vitamins Cannot Do:
- Cure macular degeneration
- Restore vision that has already been lost
A typical daily dose usually includes Vitamin C (500 mg), Vitamin E (400 IU), Lutein (10 mg), Zeaxanthin (2 mg), and Zinc (80 mg). Always chat with your doctor before starting them, but for many, this is a cornerstone of daily care, making macular degeneration self care vitamins an essential topic.
- Eye-Healthy Foods
Build your plate around:
- Lutein/Zeaxanthin: Kale, spinach, collards, and eggs help protect the macular pigment.
- Omega-3s: Foods like salmon, sardines, and mackerel support retinal structure and reduce inflammation.
- Vitamin C: Citrus fruits, peppers, and berries provide antioxidant defense.
- Vitamin E: Almonds, sunflower seeds, and spinach help protect cell membranes.
- Zinc: Oysters, beef, and beans aid in transporting vitamin A to the retina.
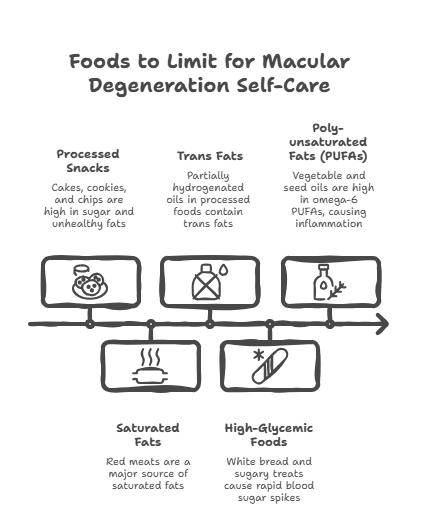
- What to Limit
Try to reduce:
- Processed snacks like cakes, cookies, and chips.
- Saturated fats are found in high amounts in red meats.
- Trans fats are often found in partially hydrogenated oils.
- High-glycemic foods such as white bread or sugary treats.
- Any Poly-unsaturated fats or PUFS, these are in all the vegetable and seed oils, avoid these at all costs.
Many countries didn’t even have AMD among their populations until the advent of the highly processed seed and vegetable oils that are high in omega 6 fat acids. These cause oxidation and inflammation.
Making thoughtful food choices is key in any macular degeneration self-care routine.
Smoking Cessation
Smoking and macular degeneration are a tough combination, and this is one area where you have huge power to change the story. Smoking doesn’t just increase your risk of developing AMD; it can double that risk, speed up progression, and make treatments (like injections for wet AMD) less effective. The good news: as soon as you stop, your body begins to repair. Within months, circulation improves, oxidative stress drops, and your eyes receive better oxygen and nutrients. That’s real, measurable macular degeneration self-care at work.
It is never too late to benefit from quitting, even if you’ve smoked for many years or already have AMD. You don’t have to do it alone. Helpful tools include:
- Quitline: Call 1800-QUIT NOW for free coaching and support
- Nicotine replacement: Patches, gum, lozenges to ease withdrawal
- Prescription medications: Your doctor can recommend medicines that reduce cravings
- Support programs: In-person or online groups that keep you accountable and encouraged
If you smoke, quitting is the single most important self-care action you can take for your eyes and your overall health. Every smoke-free day is a direct investment in your future vision and a vital part of consistent macular degeneration self-care. It’s never too late to begin a healthier chapter in your life.
UV and Blue Light Protection
Think of protecting your eyes from UV and blue light as a simple daily habit that pays dividends for a lifetime. UV damage is cumulative, meaning it builds up slowly over many years. The more protection you give your eyes now, the more you’re safeguarding your future vision principle at the heart of macular degeneration self-care.
Here’s how you can make it a simple part of your routine:
- Block UV Rays Outdoors: Always choose sunglasses labeled “UV 400” or “100% UV protection.” This ensures they block the harmful UVA and UVB rays. A wrap-around style offers even better protection by stopping light from sneaking in from the sides.
- Add a Hat: Pair your sunglasses with a wide-brimmed hat. This helps cut down on glare from above and light reflecting off surfaces like water, sand, or pavement.
- Filter Blue Light Indoors: If you spend a lot of time on computers, tablets, or phones, blue light filtering glasses can help reduce eye strain. While they don’t replace your outdoor sunglasses, they add a helpful layer of protection on screen-heavy days.
Make eye protection a reflex. Just as you’d grab a jacket on a cold day, grab your sunglasses and hat when you head outside, even when it’s cloudy. Keep a spare pair in your car or by the door so you’re never caught without them. These small habits make a big difference in preserving the delicate tissues in your macula over the long run, especially with wet macular degeneration self-care in mind.
Blood Pressure & Cardiovascular Health
High blood pressure doesn’t just affect your heart; it directly affects your eyes. When your BP is high, the tiny blood vessels that nourish your retina can become narrowed and damaged, reducing blood flow to the macula and potentially speeding AMD progression. For most people with AMD, doctors often aim for a blood pressure below 130/80, unless your healthcare team sets a different target for you.
Key ways to support healthier numbers include:
- Weight loss: Even 5-10 pounds can make a measurable difference.
- Cut sodium: Aim for less than 2,300 mg per day (check labels; salt hides everywhere).
- Move daily: About 30 minutes of brisk walking or similar exercise most days of the week.
- Manage stress: Relaxation techniques, breathing exercises, hobbies, and good sleep.
- Take medications exactly as prescribed: skipping doses can cause silent damage over time.
AMD shares many of the same risk factors as heart disease and stroke, so protecting your cardiovascular health also protects your vision. This is a vital area of macular degeneration self-care. Work closely with your primary care doctor and eye specialist to create a plan that fits your lifestyle and medical needs.
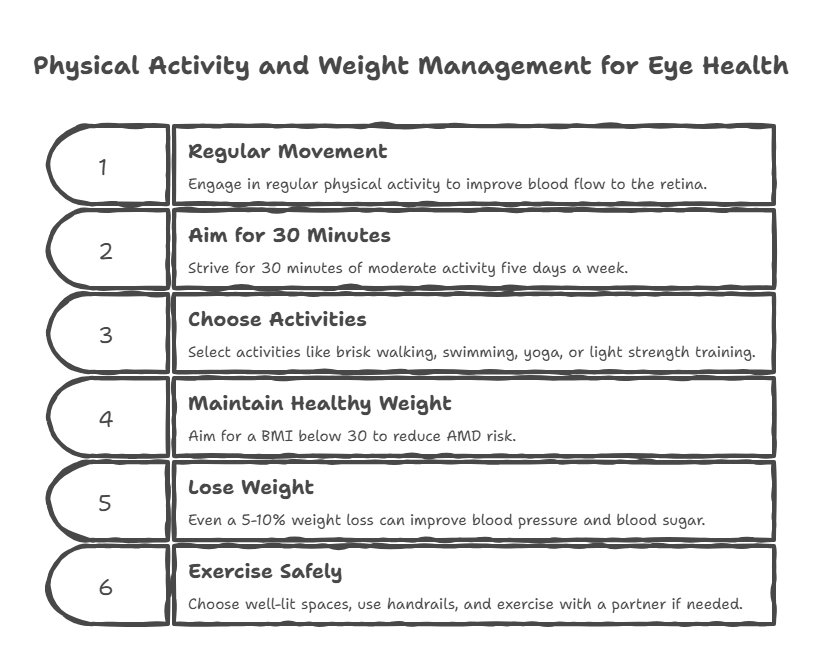
Physical Activity & Weight Management
Regular movement is a powerful tool for protecting your eyes and overall health. Exercise improves blood flow to the retina, and studies suggest it can reduce AMD risk by up to 70% when combined with other healthy habits.
Aim for about 30 minutes of moderate activity, five days a week. Good options include:
- Brisk walking
- Swimming or water aerobics
- Yoga or tai chi
- Light strength training
Your body weight also plays a role. A BMI over 30 is linked with a higher risk of AMD, but even a small change makes a difference. Losing just 5-10% of your body weight can lower your blood pressure, improve your blood sugar, and support your eye health.
Even with low vision, you can exercise safely. Choose well-lit, clutter-free spaces; use handrails; exercise with a partner; or try stationary equipment. Every bit of movement is a step toward protecting your future vision and is encouraged by self-care resources for macular degeneration.
How to Monitor Your Vision at Home
Keeping a close eye on your vision (literally!) is one of the smartest things you can do with AMD. Self-monitoring tools help you catch changes early, when treatment can be most effective.
1) Amsler Grid – Your Daily Check
The Amsler grid is a simple checkerboard pattern with a dot in the center.
How to use it:
- Wear your usual glasses.
- Hold it 12-15 inches away.
- Cover one eye, and focus on the center dot.
- Repeat with the other eye.
Watch for:
- Wavy or bent lines.
- Dark or gray spots.
- Missing or blurry areas.
If you notice ANY change, call your eye doctor immediately. Keep a printable grid on your fridge or bathroom mirror so it’s easy to use every day as part of your ongoing macular degeneration self-care.
2) Vision Tracking
Keep a small vision journal or notes in your phone to track changes. Record the following:
- Which eye is affected?
- Date and time.
- What you noticed (distortion, dim area, etc.).
Bring this journal to your eye appointments. Many smartphones also have vision or eye-check apps you can use between visits for added convenience.
3) When to Escalate
- Sudden vision change: Call your doctor right away.
- Slow, gradual worsening: Bring it up at your next visit.
- New flashes, floaters, or a curtain over vision: Seek urgent care immediately.
A Simple Tip to Remember
Early detection and consistent monitoring can make a significant difference in managing your vision and preserving your independence, especially for those focused on wet macular degeneration self-care.
Low Vision Aids for Self-Care
Low vision aids are not “giving up”; they are powerful self-care tools. By maximizing the vision you still have, you protect your independence, safety, and quality of life. In fact, about 80% of people report better daily function when they’re matched with the right devices and training, making them a key aspect of macular degeneration self-care.
- Reading & Close Work
If small print is frustrating, the right tools can bring it back into reach:
- Handheld magnifiers (3x-10x) for price tags, labels, and menus.
- Stand magnifiers for hands-free reading or crafts.
- Electronic/CCTV magnifiers that enlarge text on a screen.
- Audiobooks to give your eyes a break while still enjoying reading.
- Electronic Handheld magnifiers- these can magnify up to 32 times, often have stands built in and bright LED lights. They have filters, blocks, and lines to help you to not lose your place while reading.
- Lighting
Good lighting is just as important as magnification.
- Use task lamps with flexible arms and bright (high-lumen) bulbs.
- Most people with AMD need 2-3 times more light than they did at age 20.
- Reduce glare by adjusting the lamp angle rather than increasing brightness alone.
- Daily Living Aids
Simple adaptations make home tasks easier and safer:
- Large-button phones, talking watches/clocks
- High-contrast cutting boards for safer food prep
- Medication organizers and talking labels
- Technology & Advanced Options
- Screen magnification and text-to-speech apps for phones/computers
- Smart glasses (e.g., eSight, IrisVision) for some people with advanced AMD
- Voice assistants (Alexa, Siri) for hands-free information and reminders
Using aids early helps prevent isolation, maintain hobbies, reduce falls, and support mental health. Choosing help is a strong, proactive act of macular degeneration self-care.
Adding tools that simplify your routines is not about loss; it’s about opportunity.
Wet AMD-Specific Self-Care
Living with wet AMD means your treatment routine becomes a core part of self-care, but it’s also your strongest tool to protect your vision. Wet macular degeneration self-care revolves around regular visits, monitoring, and healthy habits.
- Treatment Compliance
Anti-VEGF injections work only if they’re on schedule. Skipping or delaying appointments can lead to rapid vision loss.
- Use calendar reminders and alarms to keep track of appointments.
- Plan transportation; you may not feel comfortable driving afterward.
- Bring a companion for support and to help you get home safely.
- Post-Injection Care
Follow your doctor’s instructions closely for a safe recovery:
- Use any prescribed drops exactly as directed.
- Avoid rubbing your eye for at least 24 hours.
- Call your doctor immediately if you notice severe pain, a significant drop in vision, or increasing redness.
It is normal to experience a few floaters or mild scratchy feelings in the first 24-48 hours; however, if you’re concerned, don’t hesitate to check with your doctor.
- Between Injections
All general AMD self-care practices remain important to maintain eye health and overall well-being:
- Follow a healthy diet, avoid smoking, control blood pressure, and protect your eyes from UV exposure as part of a dedicated wet macular degeneration self-care routine.
- Take AREDS2 supplements if recommended by your doctor; these are the main macular degeneration self care vitamins for many patients.
- Check your Amsler grid daily, and report any new distortions or dark spots immediately.
Remember, wet AMD can progress quickly, so avoid the urge to “wait and see” with new symptoms. Practicing wet macular degeneration self-care is about prompt response and consistency.
- Emotional Management
Feeling anxious about injections is very common.
- Ask about support groups Talking with others who understand your experience can be incredibly helpful.
- Consider counseling if you notice persistent sadness or depression.
And always remember this simple truth: stable vision is a win. Even keeping your sight from getting worse is a success worth celebrating. That’s why wet macular degeneration self-care deserves your focus.
Home Safety: Prevention is Self-Care
When you live with vision loss, making your home safer is a major act of macular degeneration self-care. Falls are a leading cause of injury for seniors with low vision, but many falls are preventable.
- Clear the Hazards
Walk through your home with “safety eyes.” Are there loose rugs you could trip on? Tape them down or remove them. Clear clutter from hallways and stairs. - Use Contrast
Vision loss often reduces your ability to see contrast (the difference between light and dark). You can help your eyes by creating it artificially:
- Put a dark placemat under a white dinner plate.
- Place bright, colorful tape on the edge of the stairs.
- Use a different colored toilet seat so it stands out from the floor.
- Organization
Give everything a “home.” Your keys, phone, remote, and medications should always go back to the exact same spot. This allows you to find things by habit and touch, reducing frustration, an important part of macular degeneration self-care.
Emotional & Mental Health Self-Care
Living with AMD impacts more than just your vision; it affects your emotions, identity, and daily life. Nearly 30% of people with AMD experience depression, while many face anxiety about blindness or losing independence. Vision loss is a form of grief, and feeling shock, anger, or sadness is natural. Allowing yourself to grieve is a healthy part of coping.
- Emotional Self-Care Strategies
- Stay socially connected: Regular calls, visits, or online chats help prevent isolation, which can worsen depression.
- Join AMD support groups (online or in person) to talk with people who truly “get it.”
- Consider professional counseling, especially with a therapist who understands chronic illness or vision loss.
- Adapt your hobbies with low vision aids so you can keep doing what you love, even if it looks different now.
- Set realistic goals (e.g., “Read 10 minutes with a magnifier”) and celebrate each success.
- Practice self-compassion: Talk to yourself the way you’d talk to a friend in the same situation.
- Helpful Resources
- Depression screening tools (like short questionnaires) to check your mood.
- A therapist experienced in chronic illness or disability.
- Support groups for AMD or low vision peers.
- A crisis line if you ever feel unsafe or overwhelmed.
Your emotional well-being is just as important as your eye injections, your macular degeneration, self-care vitamins, or supplements; it’s all part of caring for you.
Your Daily Self-Care Routine
It can feel overwhelming to think about all these steps for macular degeneration self-care. Here is a simple daily schedule to help you fit it all in.
Morning
- Take your AREDS2 supplement with breakfast. These macular degeneration self care vitamins are important for many patients.
- Do your Amsler grid check (one eye at a time).
- Take any blood pressure meds.
- Move your body for 15-30 minutes.
During the Day
- Wear your sunglasses and hat whenever you go outside.
- Use bright task lighting for reading or cooking.
- Use your magnifiers without hesitation as part of your macular degeneration self-care routine.
- Eat a lunch rich in greens or colorful veggies.
Evening
- Jot down any vision changes in a notebook.
- Tidy up walkways (shoes, cords) to prevent falls at night.
- Relax with an audiobook or music to give your eyes a rest.
Weekly Check-In
- Prepare meals using eye-healthy ingredients like leafy greens, colorful vegetables, and omega-3-rich fish.
- Review your appointment calendar to ensure you don’t miss any injections or eye exams, which are especially vital for wet macular degeneration self-care.
- Check your stock of supplements and low vision aids to stay prepared.
- Try to join at least one support group or social activity each week to connect with others and maintain emotional well-being.
When Self-Care Isn’t Enough
Sometimes, even when you’re doing everything “right,” it can feel like it’s not enough, and that’s okay. Reaching out for extra help is part of good self-care, not a sign of failure. Sometimes, macular degeneration self-care needs the support of your care team, too.
- Signs You Might Need More Support
It’s time to seek professional guidance if you notice:
- Worsening Vision: Your sight seems to be declining despite your self-care efforts.
- Emotional Distress: Feelings of depression, anxiety, or fear make it hard to get out of bed, enjoy activities, or care for yourself.
- Difficulty with Daily Tasks: You struggle to do essential things safely, like cooking, managing medications, or getting around your home.
- Isolation: You feel withdrawn and are avoiding people or hobbies you once enjoyed.
- Feeling Overwhelmed: You’ve missed medical appointments, like injections or eye exams, because it all feels like too much.
- Who Can Help?
- Your Ophthalmologist: Contact them right away for any new or worsening vision problems as part of attentive macular degeneration self-care.
- A Low Vision Specialist: They can help you get the most out of your remaining sight with updated glasses, magnifiers, and other strategies.
- A Mental Health Professional: A therapist can offer support for the depression, anxiety, or grief that often comes with vision loss.
If something feels “off,” please don’t wait. Getting help earlier almost always leads to better results for your vision, your safety, and your peace of mind.
Remember, needing more support doesn’t mean you’ve done anything wrong. It just means you’re ready for the next step in caring for yourself, and you deserve all the help available to support your journey with macular degeneration self-care.
Conclusion
Managing macular degeneration is a journey of small, consistent steps. While you can’t control everything, you have more influence than you might realize. A solid self-care routine, including the right vitamins and proactive habits for wet or dry AMD, can make a real difference.
You don’t have to overhaul your life today. Start with one small change. This week, maybe you can focus on wearing sunglasses and taking your vitamins. Once that’s a habit, you can add another step, like a daily Amsler grid check.
You can do this. By prioritizing these daily habits, you’re protecting your independence and honoring the vision you have.
Take the Next Step
- Schedule an Exam: If you’re overdue, call your eye doctor today.
- Check Your Vitamins: Ask if an AREDS2 supplement is right for you to support long-term vision.
- Get Equipped: Explore our Self-Care Products designed to support your safety and independence.
As a Low Vision Specialist I can tell you that getting the right devices to help you keep your independence can really help keep your spirits high and your depression at a minimum. Vision loss isn’t fun but you don’t have to do it alone and without a fight.
A recent patient told me that getting his bioptic telescope glasses “had changed his life in ways he thought weren’t possible anymore” they helped him get his drivers license back!
Frequently Asked Questions
Q1: Can self-care stop macular degeneration progression?
No, macular degeneration self-care can’t cure or fully stop AMD, but it can slow progression and help protect remaining vision, especially in early and intermediate stages.
Q2: What vitamins should I take for macular degeneration?
If you have intermediate or advanced dry AMD, ask your doctor about an AREDS2 supplement (vitamins C and E, lutein, zeaxanthin, zinc, and copper). Don’t start without medical advice; these are the main macular degeneration self care vitamins recommended in many macular degeneration self-care guides.
Q3: Is self-care different for wet vs dry AMD?
Core habits are the same (diet, no smoking, UV protection, blood pressure control), but wet AMD also requires strict injection compliance and rapid reporting of new symptoms. Wet macular degeneration self-care includes all these basics plus additional monitoring.
Q4: How often should I check my Amsler grid?
Check daily, one eye at a time. Call your eye doctor immediately if you see new distortion, dark spots, or missing areas as part of vigilant macular degeneration self-care.
Q5: Will low vision aids help my macular degeneration?
They don’t treat the disease, but they maximize remaining vision, improve independence, and reduce accidents and frustration. Low vision aids are an important part of macular degeneration self-care.
Q6: Can I reverse macular degeneration with diet?
No, but an eye-healthy diet + AREDS2 (if appropriate) can help slow progression and support overall eye and heart health. Good nutrition is a cornerstone of smart macular degeneration self-care.
Q7: Should I stop driving with macular degeneration?
It depends on your vision and local laws. Your eye doctor can test your vision and advise whether driving is still safe and legal for you, based on macular degeneration self-care considerations.
Q8: How much exercise do I need for AMD self-care?
Aim for about 150 minutes per week of moderate activity (like brisk walking), with your doctor’s approval. Staying active supports your general and macular degeneration self-care goals.
Q9: Can I drink alcohol with macular degeneration?
Light to moderate drinking may be acceptable for some people, but heavy alcohol use is harmful. Ask your doctor what’s safe for you as part of your overall self-care strategy.
Q10: When should I start using low vision aids?
Earlier than you think. Start as soon as vision changes begin affecting reading, hobbies, or safety. Early use prevents isolation and helps you adapt more easily, according to most macular degeneration self-care specialists.