Inherited retinal diseases are rare conditions which, left untreated, can lead to permanent vision loss or blindness. Today at AEVR’s Congressional Briefing we will focus on these less well-known, but equally awful diseases.
Disease transmission occurs through an individual gene mutation and only affects those carrying its altered chromosome.
Retinitis Pigmentosa
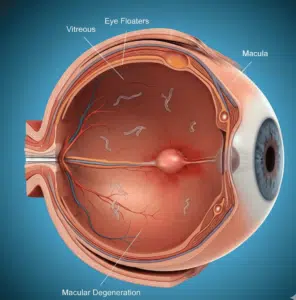
RP (retinitis pigmentosa) is an inherited condition that affects the retina – the light-sensitive tissue at the back of the eye – in early childhood, often leading to night blindness and limited field of vision. Over time, as the disease worsens it becomes harder and harder to see details and colors; some even become legally blind as time progresses. It may be passed from parent to child via dominant inheritance pattern with just one gene mutation needed; it also occurs as an X-linked recessive form which usually affects males.
Electroretinogram tests can easily identify this condition through flashes of light that illuminate the patient’s eyes and measure electrical activity in their photoreceptor cells; people suffering from Retinitis Pigmentosa tend to exhibit lower electrical activity levels compared to those without it, signaling their cells are starting to die off.
Video magnifiers can help those living with Rett Syndrome improve their hands and eyesight when doing activities requiring close attention, such as threading a needle or reading. People may also benefit from brighter lights, increasing contrast levels in their environment, or wearing dark glasses to enhance contrast levels and decrease eye strain. New treatments are being developed to slow or stop further vision loss – Rare Disease Registries help speed clinical development of new therapies and provide easier access to diagnostic methods and follow up services.
Nevi
Uncommon eye diseases still have the ability to cause vision loss and blindness for many patients. On May 25th, AEVR hosted a Congressional Briefing dedicated to less-common diseases that impact fewer individuals such as Age-Related Macular Degeneration or Diabetic Retinopathy yet still pose threats to many Americans’ health.
At this Congressional Briefing, Ben Shaberman, Vice President of Science Communications of the Foundation Fighting Blindness discussed research advances funded by the National Eye Institute into rare retinal disease research; while Dan Ignaszewski of AEVR provided information regarding advances in Thyroid Eye Disease.
Nevi are visible, long-term skin lesions caused by genetic mosaicism that manifest as visible lesions that reflect genetic mosaicism. Nevi can be both malignant (neoplastic) and non-malignant (non-neoplastic), acquired or hereditary, with various symptoms including vision loss, cataracts, double vision, swelling of eyelids and light sensitivity.
As these eye conditions are relatively rare, healthcare professionals find it challenging to detect and monitor them effectively. One method that could aid this effort is fundus autofluorescence imaging (FAF). FAF is a fast, non-invasive imaging technique which detects inflammation in ocular tissue – making it particularly helpful when monitoring posterior and panuveitis, two serious conditions which affect central retina and cause progressive decrease in visual acuity for both eyes.
Bietti’s Crystalline Dystrophy
Bietti’s Crystalline Dystrophy (BCD) is an autosomal recessive tapetoretinal degeneration characterized by small sparkling crystals in the retina and corneal limbus, eventually leading to progressive chorioretinal atrophy with symptoms including night blindness and reduced visual acuity, as well as paracentral scotomas in the visual field enlarging over time. BCD is thought to be caused by mutations of the CYP4V2 gene which encodes for protein involved with fatty acid metabolism within retinal pigment epithelium/choroid cells – over 100 mutations have already been found so far among patients diagnosed.
People living with BCD usually notice decreased vision in their teens or twenties. Common symptoms of BCD include difficulty seeing in dim lighting (night blindness), reduced sharpness of vision, and loss of areas of peripheral (peripheral) vision – most frequently side (peripheral). Sometimes central vision may also be affected and eventually central acuity reduces to below legal blindness by their third decade of life.
Initial misdiagnosis often delays diagnosis, contributing to its delay. BCD may be misunderstood as other retinal diseases such as gyrate atrophy, cystinosis, Sjogren-Larrson syndrome and primary hereditary hyperexcystinuria; or metabolic disorders like secondary hyperoxaluria; but molecular genetic testing using next-generation sequencing can help establish genotype-phenotype correlation when clinical features alone cannot do the trick.
Bell’s Palsy
Bell’s Palsy is a condition in which one side of the face experiences muscle weakening or paralysis due to damage to the nerve responsible for controlling movement of facial muscles (the seventh cranial nerve or facial nerve).
A neuroma occurs when there is swelling where a nerve passes through bones of the skull. It may be brought on by viral infection such as herpes simplex or varicella zoster, more frequently seen among people who are pregnant or living with diabetes, but can affect anyone of any age.
Occipital tension typically affects just one side of the face, yet can sometimes result in other symptoms, including taste changes or sound distortion. It can be extremely distressful; many patients find their symptoms worse at night but often improve within several weeks or months.
Diagnosing Bell’s Palsy can be difficult, but it is vital that if one side of your face droops that you see a doctor immediately in order to rule out more serious conditions like stroke. Most cases will recover without treatment within three weeks and often completely within six months.
Anopthalmia & Micropthalmia
Congenital condition wherein one or both eyes are abnormally small at birth. It may affect both eyes unilaterally or bilaterally. The optic nerve and chiasm may be absent in severe cases; and in addition, the clear front covering of the eye (cornea) may be abnormally curved resulting in abnormal vision; often associated with cataracts.
Gene mutations that interfere with early ocular development often cause this condition. People born with anophthalmia and extreme microphthalmia often fall under one of several genetic syndromes such as Goldenhar Syndrome (sporadic; anophthalmia, ear defects, cleft lip/palate, facial macrosomia), Fraser Syndrome (autosomal recessive; anophthalmia, tracheal atresia, genital anomalies, heart defect ventriculomegaly syndactyly), or VSX2 Syndrome.
Severe microphthalmia may be associated with severe symptoms, including esophageal atresia and an unusual connection between the esophagus and trachea (tracheoesophageal fistula). Genital abnormalities often accompany SOX2 anophthalmia syndrome; undescended testes (cryptorchidism) or an unusually small penis (micropenis).
People affected by anophthalmia have mild to severe vision loss in both eyes, usually present from birth but sometimes detected during gestation through prenatal ultrasound or genetic testing. A newborn who exhibits either extreme microphthalmia or anophthalmia will require evaluation by both a pediatric ocularist and an oculoplastic surgeon in order to ensure proper care is being administered; it’s imperative that they work collaboratively in creating the necessary team of experts who provide necessary support and therapy services.
Glaucoma
Glaucoma is a group of disorders that damage the optic nerve that connects your eyes to your brain. It typically happens when intraocular pressure (IOP) becomes higher-than-normal levels (a condition known as intraocular hypertension). Over time, this higher pressure damages the optic nerve gradually and leads to irreversible vision loss if untreated; it is currently the second-leading cause of blindness worldwide and second in America (second only to cataracts). While anyone at any age may be susceptible, adults over 60 are particularly susceptible.
Open-angle glaucoma is the most prevalent form of the disease and usually remains symptom-free until later stages. A less prevalent variant called acute angle-closure glaucoma develops when your eye fails to drain inner eye fluid efficiently, leading to severe eye pain, headaches, blurry vision and nausea – it can even be life threatening!
Although rare diseases aren’t contagious, regular visits to an ophthalmologist are nonetheless necessary to ensure your eyes and vision stay in top condition. By detecting potential problems with your vision early, an eye doctor can prescribe preventive medication which will improve quality of life and ultimately ensure continued independence for years.