High blood pressure (hypertension), also known as high vascular tension, damages blood vessels throughout the body – including retinal blood vessels. Studies have indicated a correlation between systemic blood pressure and retinal blood vessel changes.
Blood pressure-lowering medication and lifestyle modifications may help control systemic hypertension. The goal should be to keep blood pressure below 140/90 mmHg.
Grade 1
High blood pressure can damage the delicate blood vessels in the retina (the light-sensitive layer at the back of your eye), potentially resulting in hypertensive retinopathy – leading to vision loss or serious cardiovascular consequences if left untreated.
Hypertensive retinopathy in its early stage is marked by small and scattered hemorrhages in the retina that appear as small spots or flames and reddened blood vessels, making diagnosis often difficult; fundus photography may help identify its early signs.
Chronic elevation of blood pressure triggers local autoregulatory mechanisms within retinal arterioles to initiate narrowing and vasospasm, decreasing blood flow. Over time, endothelium cells infiltrate blood vessel walls leading to degradation. Over time this leads to formation of fibrovascular stroma as well as leakage through blood-retina barrier allowing leakage of fluid into retina. Ophthalmoscopically this results in retinal arteriolar narrowing with copper or silver hued blood vessels, changes at arteriovenous crossing points narrowing or changes, narrowing arteriovenous crossing changes as well as deflection distal to these crossing points (also referred to as ‘AV nipping’).
These changes in blood vessel structure aren’t considered risk factors for coronary artery disease and may not correspond with changes in brachial-ankle pulse wave velocity (baPWV) or aortic root diameter, yet can provide insight into future cardiovascular events among people living with hypertension.
Patients diagnosed with grade 1 hypertensive retinopathy should meet with their primary care physician to discuss lowering their blood pressure and lifestyle measures that could assist in controlling it, including diet, exercise, salt reduction, alcohol limits reduction and visits to their ophthalmologist for regular check-up visits.
Hypertensive retinopathy can be effectively managed with long-term blood pressure management, and in certain cases fluorescein angiography. Patients will benefit from ongoing follow up appointments with their ophthalmologist in order to monitor treatment effectiveness as well as progression towards further hypertensive stages.
Grade 2
Hypertension damages blood vessels of the retina (the light-sensitive structure at the back of the eye). Over time, these damaged blood vessels bleed or leak fluid into nearby tissue and this leaking may lead to blurry vision as well as headaches or eyestrain. At first, symptoms may not be noticeable and diagnosis should come with routine visits to an eye care professional; however double vision or dim vision, blurry or fuzzy vision, sudden symptoms or double or dim vision may indicate that blood pressure levels have reached dangerously high levels and require urgent medical intervention.
Eye care professionals will first assess whether an individual has systemic high blood pressure by conducting a complete history review and physical exam of their patient. Furthermore, an eye professional will check for signs of ocular hypertension; its symptoms being changes or leakage in retinal blood vessels that lead to vision loss particularly near the central area (macula). Although symptoms may not always be evident at this stage of disease progression, they become increasingly noticeable as more blood vessel leakage increases.
Grade 1
Early signs of ocular hypertension often include small blood vessels in the retina exhibiting bluish tinting and narrowing, known as macular ischemia and indicative of untreated high blood pressure. Furthermore, small capillaries within the retina may swell up or become cotton-wool like. An eyescare professional will identify such conditions using dilated fundoscopic exams before prescribing an antihypertensive regimen of medication to treat it.
Grade 2
As part of ocular hypertension’s second stage, some small capillaries will begin leaking blood or fluid. Leakage typically appears bluish-toned on fundoscopic examination, and can often be recognized by their characteristic “copper or silver wire” appearance. Leaks can cause swelling of surrounding retinal structures and distortion or blurriness to vision; sometimes enveloping optic nerves and macular areas leading to decreased visual acuity.
Grade 3
Long-term high blood pressure can damage retinal blood vessels in the eye, known as hypertensive retinopathy. This condition can progress to affect vision in significant ways – symptoms may include blurry vision, decreased visual acuity and eyestrain; diagnosis typically requires dilated fundoscopic exam. Patients suffering from hypertension should see their eye doctor regularly to monitor and ensure control over their blood pressure levels.
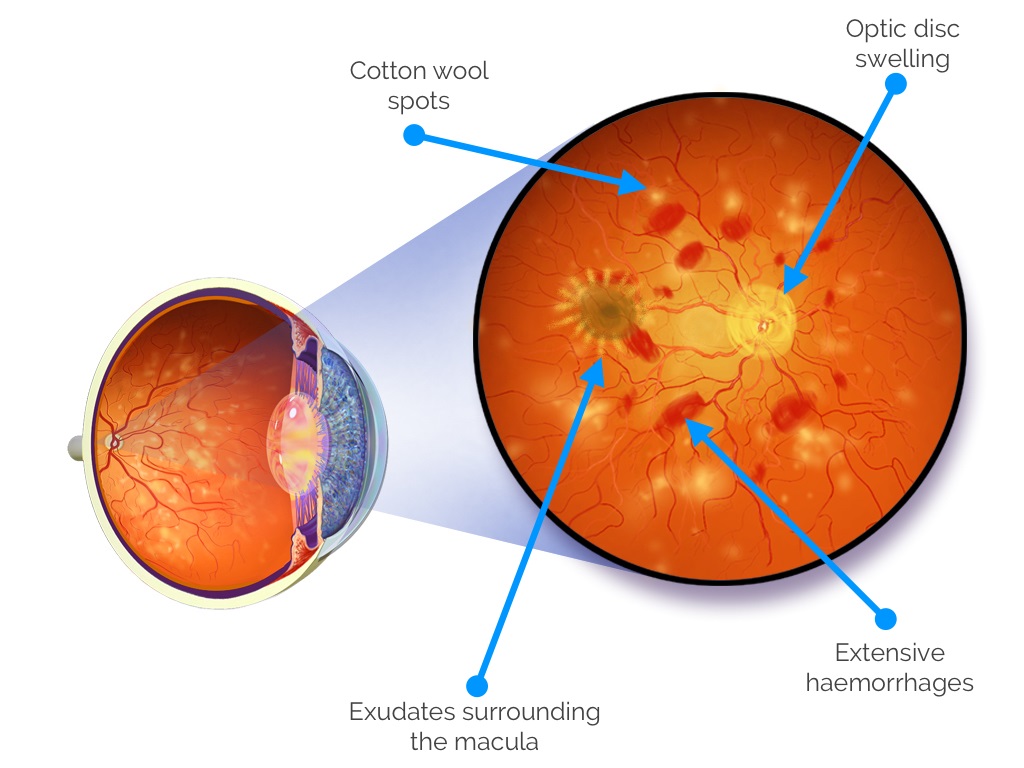
Hypertensive retinopathy is classified into four grades with increasing severity: grade one involves mild generalized retinal arteriolar narrowing; grade 2 includes more severe generalized narrowing with focal areas of arteriolar narrowing plus arteriovenous (AV) nicking; grade 3 features hemorrhages, microaneurysms, hard exudates and cotton wool spots; while grade 4, also known as accelerated or malignant hypertensive retinopathy, contains all features from grades 1-4 plus optic disc swelling (papilloedema).
Research has demonstrated a correlation between eye changes and systemic blood pressure levels and their severity. Mild hypertensive retinopathy such as retinal arteriolar narrowing, AV nicking and microaneurysms is weakly associated with cardiovascular disease in general populations; moderate retinopathy — such as flame-shaped or blot haemorrhages, hard exudates or cotton wool spots — strongly linked with subclinical or clinical cardiovascular diseases; the Beaver Dam Eye Study further demonstrated this correlation by showing persons whose blood pressure wasn’t properly managed had more visible signs of retinopathy than those whose blood pressure was properly managed on medication had more visible signs.
Poorly managed blood pressure may also have serious repercussions for other parts of the body such as kidneys, blood vessels and the brain. Therefore, hypertension should be addressed immediately in order to prevent heart attack, stroke and other complications. When treating patients with high blood pressure, medication such as beta blockers, diuretics calcium channel blockers or angiotensin converting enzyme inhibitors are typically employed; regular follow up appointments must also take place between eye doctors and primary care physicians in order to ensure blood pressure control is effective.
Grade 4
Hypertensive Retinopathy occurs when high blood pressure damages delicate blood vessels in the eye. Retinal blood vessels thicken and narrow, restricting how much oxygen reaches the retina from flowing in and out, ultimately leading to serious vision problems in time. Anyone experiencing these symptoms should seek medical advice immediately – hypertensive Retinopathy requires immediate medical intervention in order to ensure healthy eye circulation.
As hypertension worsens, retinal blood vessels thicken and narrow further, allowing more fluid to leak out through them and cause symptoms including flame-shaped and blot hemorrhages, cotton wool spots and hard exudates in the center of the retina known as macula. If left untreated, severe cases could result in swelling of optic nerve or of macula area of retina leading to worsening vision.
Retinal blood vessels are usually controlled through an automatic mechanism known as autoregulation, where vessels either narrow or widen depending on bloodflow. High blood pressure may, however, disrupt this process by permanently thickening retinal vessels that allow oxygen into the retina via bloodflow.
Keith and Scheie grading systems were once widely utilized to classify changes in retinal blood vessels among patients with hypertension; however, recent evidence has demonstrated their limited correlation with both baPWV and aortic root diameter values; consequently, most experts do not advise routine ophthalmoscopic examination for such individuals.
Hypertensive retinopathy can be treated by taking steps to lower blood pressure gradually and responsibly, including adopting healthier lifestyle habits and cutting down on salt consumption. Patients should visit their doctor regularly for check-ups as this treatment aims to prevent further blood vessel damage both within the eye and elsewhere in their bodies.
Most patients suffering from hypertensive retinopathy will regain their vision with time, while some will require medication like diuretics, angiotensin converting enzyme inhibitors or beta blockers to treat blood vessel damage. More serious cases may require laser surgery as a solution.