Diplopia is a common neurological complication and should be evaluated closely to ascertain its cause. Monocular diplopia should also be carefully considered when diagnosing symptoms.
Typically, the direction of gaze that produces worse diplopia helps identify the offending extraocular muscle(s). Ocular motility testing should also be undertaken in order to detect abnormalities (e.g. disconjugate eye movement or nystagmus). Isolated single cranial nerve palsies without other symptoms may resolve spontaneously.
Causes
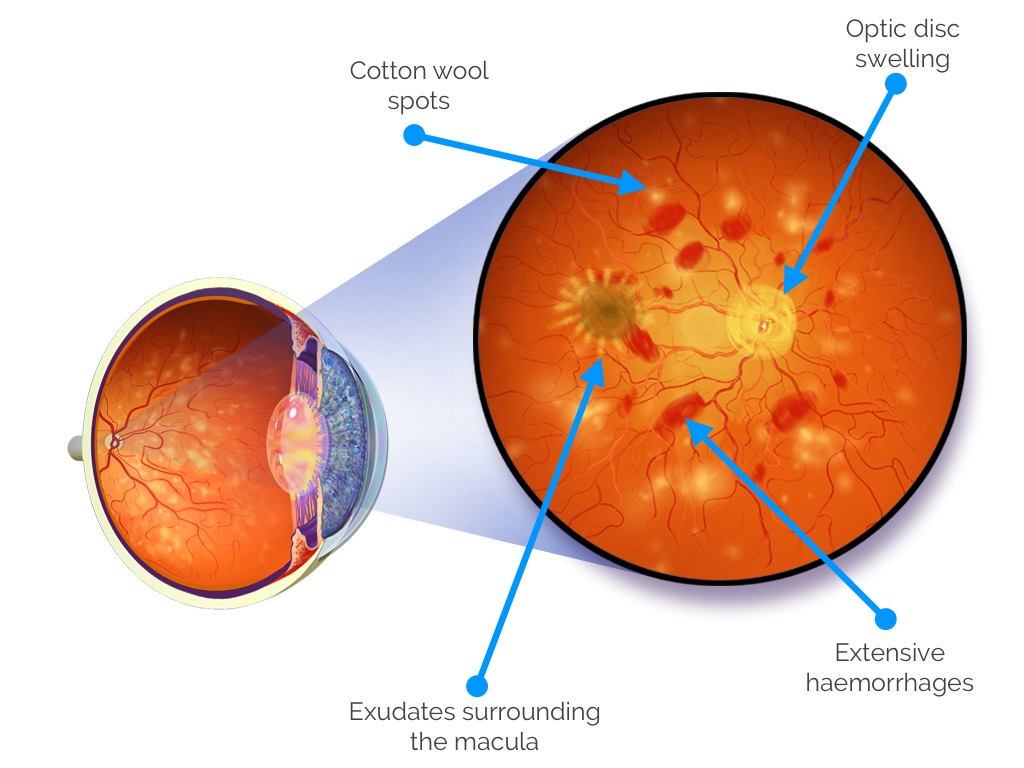
Idiopathic intracranial hypertension, or IIH, refers to an increase in normal pressure within the skull that doesn’t result from mass lesions or hydrocephalus. Suspect IIH when visual disturbances (double vision) appear without explanation while brain imaging studies such as an MRI are normal; associated with high serum cholesterol levels and increased blood pressure especially among women in childbearing age.
An extensive history and examination are key in diagnosing diplopia. Noting its frequency, type, location and other aspects are vitally important; including whether the double images are constant or intermittent and involve either one or both eyes, as well as whether they appear horizontal, vertical or obliquely. Also helpful are observations as to whether they disappear when either eye is covered; as well as whether its effects worsen with certain head movements like looking upward or downward – this information could reveal which extraocular muscle(s) could be at play.
Neurological examination should include taking a detailed history of any recent trauma or surgery, evaluating for cranial nerve palsies and orbital fractures, ocular motility testing (noting any abnormal eye movements such as an outward turning of lid) or inward turning (entropion). Lumbar puncture and cerebrospinal fluid testing may be recommended if elevated intracranial pressure and no obvious cause is suspected for diplopia.
Diplopia treatment often relies on its source, including better blood sugar management if associated with diabetes or treatment with antihistamines to address vision impairment. Medication prescribed for myasthenia gravis or other autoimmune conditions may also help improve vision, while structural causes of diplopia such as orbital fractures or strabismus are typically managed through physical therapy, medication and surgery. Psychological support and education can also play a key role in helping adjust to changes in perception and manage everyday activities. A multidisciplinary approach may often be necessary, including visits from ophthalmologists, neurologists, endocrinologists and maxillofacial surgeons. Diplopia can significantly diminish quality of life; thus prevention strategies include maintaining a healthy weight, managing chronic conditions like diabetes and high blood pressure, as well as regular eye exams to identify any potential problems.
Diagnosis
Double vision diagnosis requires a comprehensive history and exam by an eye care provider, in which one eye will be covered while re-fixation movements are examined on both. These reveal whether the deviation of one ocular (strabismus) occurs constantly (manifest/tropia), or only when covered (latent/phoria).
Additionally, visual fields should be assessed and the optic fundus inspected to evaluate diplopia as soon as it appears suddenly or subtly. It’s especially important in cases of sudden or insidious onset to determine whether diplopia is bilateral, binocular, monocular or intermittent and whether head movements cause it. Furthermore, it would be wise to identify any associated headache symptoms, their severity and whether they’re associated with vision changes.
If the cause of diplopia is suspected to be neurological, specialized imaging should be sought out as soon as possible. An MRI brain scan is often the best way to identify and treat this condition; an ophthalmologist will also conduct an eye exam in order to detect any abnormalities that might exist within the pupil or eyelid position.
Monocular diplopia symptoms often stem from intraocular pathology; however, in rare instances they could also stem from cerebral sources, such as lesions of Brodmann’s area nineteen, frontal eye fields or cerebellum. Diplopia must be treated by diagnosing and treating its cause, so in cases such as Graves disease it’s necessary to perform thyroid tests such as TSH and T4 levels to make sure your thyroid gland isn’t overactive. Myasthenia gravis or multiple sclerosis patients should undergo blood work to check for these disorders, and be closely monitored for symptoms of relapse as well as signs or symptoms of spinal cord compression or herniated discs, prompt treatment can often prevent further damage and improve prognosis for a full recovery; for most of these individuals, their diplopia will resolve itself within weeks or months, enabling them to resume regular vision once more.
Treatment
Diplopia should be treated by identifying and treating its root cause. If diabetes is to blame, better managing of this disease may improve vision; surgery may be required to remove brain tumors; while for neurological conditions the appropriate therapy will depend on each disorder. In general, those experiencing hypertension diplopia should undergo periodic ophthalmic evaluations to monitor the condition and ensure it doesn’t return.
Timing of diplopia’s onset can provide valuable clues as to its cause. Sudden or abrupt appearance is typically cause for immediate investigation; gradual development less so. Furthermore, diplopia that worsens with certain directions of gaze should be evaluated further for possible cancerous lesions or abnormalities.
An extensive history and neuroophthalmic examination can reveal many of the underlying causes of diplopia. An important step is gathering a complete family history as some conditions, like familial polyposis, can have genetic components. Furthermore, reviewing medications could also prove invaluable in pinpointing possible culprits behind diplopie.
As part of a thorough neurological exam, in addition to history and neuroophthalmic exams, a thorough neurological exam should also take place. An examiner should ask the patient to follow a finger with each eye; looking upward, downward, diagonally to either side and then towards their nose (convergence). Furthermore, visual field testing must also take place during this assessment.
Neuroimaging with MRI is usually preferred, although CT may also be utilized. When diagnosing orbital or cranial nerve palsies, careful ophthalmic evaluation can often help delineate their deficit and determine whether it has progressed into pupil involvement. MRI can also detect other abnormalities like aneurysms, tumors or infections within the orbit. Surgery may be used to address diplopia; whether that means placing prisms into glasses, removing orbital masses or initiating endovascular treatment of ruptured aneurysms.
Prevention
Hypertension is a chronic and progressive cardiovascular condition with many causes. Many individuals remain unaware that they have it, placing them at risk of myocardial infarctions, stroke, congestive heart failure and renal disease. Therefore it is vital to educate individuals on the importance of regularly monitoring and reaching optimal blood pressures for best health.
Prevention options for diplopia may include controlling high blood pressure, avoiding medications that could cause hypotension, consulting ophthalmologists or neurologists when necessary, following recommended diet and exercise routines, protecting themselves with appropriate eye protection, managing chronic diseases such as diabetes adequately and seeking psychological support and positivity from friends or family members. While diplopia can be debilitating and often disabling condition, appropriate treatments can enable individuals to lead productive lives.