Cotton wool spots (CWS) can be an early indicator of systemic health problems that should not be ignored. CWS may lead to severe retinopathy or increase cardiovascular disease risk significantly.
Blurred vision can often be found among those suffering from diabetes who have damaged blood vessels that leak fluid or lipids into the retina and cause blurry vision. They’re also commonly observed among AIDS patients.
Causes
Cotton wool spots, or retinal puffy spots, are puffy white areas found on the retina – the light-sensing layer at the back of the eye that detects light. Cotton wool spots occur when small blood vessels become blocked off from carrying blood to retinal nerve fibers, leading to swelling on their surfaces as intracellular substances cannot be cleared away by axons and vision becomes clouded over. They typically do not cause pain and will go away once their source has been treated – typically it takes just weeks! Cotton wool spots should also vanish once their causes have been resolved.
Cotton-wool spots are most frequently caused by diabetes and hypertension, which both compromise small blood vessels in the retina. This leads to macular edema – where fluid and lipid leak out from damaged vessels onto retinal nerve-fibre layer – creating the puffy white spots seen here. They may also appear due to collagen (vascular) diseases including systemic lupus erythematosus; carotid artery disease with emboli; thoracic aortic stenosis; pulmonary edema; radiation retinopathy; anemia; leukemia; Papilledema; and AIDS.
Cotton-wool spots may recur if their underlying cause remains untreated, which means regular eye exams and careful management of diabetes-related factors (e.g. glucose and blood pressure control). To effectively address cotton-wool spots, diabetic patients need to manage glucose and blood pressure control in their treatment plans to manage this complication.
Studies conducted over the years have confirmed that COVID-19 does not directly impact retinal health in patients hospitalized for severe pneumonia or other illnesses that require hospitalization in an intensive care unit, including findings such as scattered retinal hemorrhages and cotton-wool spots observed upon fundus examination are not caused by COVID-19 itself but instead stem from preexisting conditions like inflammation states, hypotension or generalized hemodynamic instability and increased inflammation response that often accompany these patients who were then admitted into ICU care.
Symptoms
A 49-year-old woman presented with a single, white area of superficial opacification overlying the retinal vessels in her left eye, with no history of systemic disease and reporting vision acuity of 20/20 in both eyes. On ophthalmic evaluation, it was noted that her optic nerve head appeared well perfused with normal cupping; macular disk thickness appeared flat without evidence of diabetic or hypertensive retinopathy; no sign was noted on fundus photography or fluorescein angiography either.
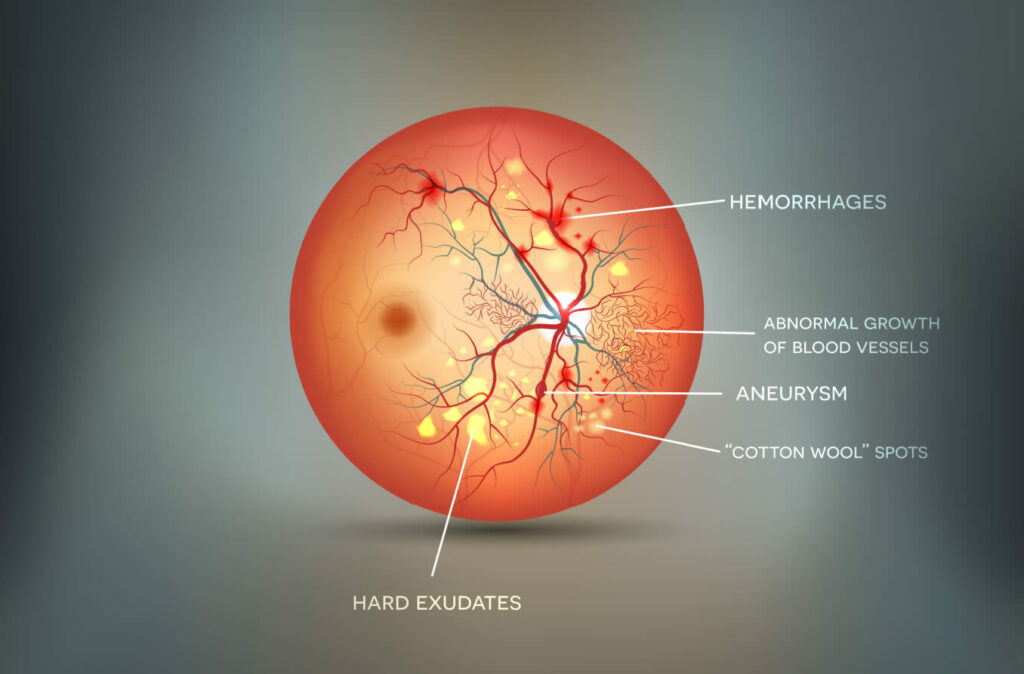
Cotton wool spots, commonly known as soft exudates or cystoid bodies, are small areas of whiteness on the retina caused by capillary infarction and are associated with conditions that affect blood vessels – such as diabetes or hypertension – leading to retinal infarction and subsequent whitening in certain spots of retinal nerve fibers. They do not cause disease themselves but may serve as indicators of more systemic health issues such as diabetes and hypertension, or be associated with conditions affecting them such as macular oedema, haemorrhages, glaucoma and even neovascularization in some cases.
Cotton wool spots were not found to be associated with COVID-19 directly; however, they could be an indicator of more serious medical conditions and should be evaluated quickly.
When patients present with symptoms related to the COVID-19 outbreak, it’s essential that we take their entire medical history into account. Preexisting conditions like giant cell arteritis could have played a part in contributing to these complications.
Giant cell arteritis (GCA) is an eye condition whereby inflammatory cells attack the vasculature of both retina and optic nerve. Ophthalmologists can easily diagnose this condition based on constitutional symptoms and an elevated Westergren ESR rate; corticosteroids can then be prescribed in order to preserve vision while clearing away cotton wool spots from affected patients.
Diagnosis
Cotton wool spots, or retinal spots, are white or grayish areas on the retina (the layer of light-sensing cells lining the back of the eye). These puffy areas are caused by small vessel occlusions that obstructing nerve fiber layers and lead to swelling within them; often associated with conditions that affect blood vessels such as diabetes and hypertension.
Spots on an eye exam signal a medical condition that must be assessed and managed, rather than simply ignored. They rarely interfere directly with vision but may recur if not managed effectively. The first step in diagnosing CWS is reviewing patient history as well as conducting an eye examination that includes dilated fundus exams to detect spots.
A 40-year-old male presented to his eye care provider with complaints of new floaters. On examination, visual acuity was 20/20 in both eyes. Dilated fundus examination of his right eye revealed wide-spread retinal hemorrhages including cotton wool spots and some white-centered hemorrhages (Figure 1). On inspection of his left eye was found vitreous hemorrhage inferiorly and preretinal hemorrhage inferonasally (VHI).
This case illustrates the changes typically associated with diabetic retinopathy. Diabetics develop this eye condition due to damage to blood vessels that leads to leakage of fluid from retinal capillaries causing exudates – an extremely painful condition. As part of their full examination by their physician, patients should undergo a comprehensive workup. This should include fasting blood glucose and antinuclear antibody levels as well as comprehensive metabolic panel and electrocardiogram with echocardiogram measurements. Evaluation should also include carotid duplex ultrasound, inflammatory markers and laboratory studies to evaluate cardiovascular systems, such as cholesterol and homocysteine level analysis. Testing should be undertaken immediately as treatment of the root cause can stop further progression of vascular changes and complications. Patients should visit their ophthalmologist regularly for care monitoring.
Treatment
Cotton-wool spots (CWS) are coagulated exudates of plasma and fibrin that represent focal areas of hypoxia. Clinically, they manifest themselves as localized areas of retinal whitening or as hyperreflective foci on optical coherence tomography (OCT). CWS may occur alone or along with macular edema; when present alongside macular edema they show as areas with thinner inner retinal layers on OCT cross sections.
Ophthalmologists are often the first to detect these features, and it’s essential not to ignore them. Though not directly threatening vision, their presence indicates systemic medical issues with serious ramifications for health and can indicate progression into more severe forms; so it is crucial that patients with CWS undergo a full workup in order to ascertain its source.
Cotton-wool spot formation is often associated with diabetes and high blood pressure, and serves as an early marker of diabetic retinopathy severity. More than eight cotton-wool spots is a strong indicator that proliferative diabetic retinopathy will develop; additionally there’s a correlation between cotton-wool spot numbers and length of diabetes as well as its control levels and longevity of disease.
Other vascular conditions can also contribute to the formation of CWS. Central retinal vein occlusion (CRVO) often results in these spots appearing and is frequently accompanied by diffuse hemorrhages around the periphery of the fundus and “blood and thunder” appearance on ophthalmoscopy. Furthermore, its formation can increase your risk for coronary artery disease and stroke.
Giant cell arteritis (GCA) may also contribute to the formation of CWS, with lesions often being the first sign. Fluorescein angiography may then be used to demonstrate concomitant choroidal ischemia; GCA treatment typically includes cyclophosphamide and prednisone as anti-inflammatories; however, even when treated appropriately long-term sequelae such as choroidal neovascularization or macular edema are likely.