An article should provide useful information to its reader, while still meeting its purpose in an engaging and accessible way. Its tone will depend on both its subject matter and who the target audience is.
1. Pterygium
Pterygium (pronounced Tuh-RIJ-ee-um) is an eye growth that starts on the white part of your eyeball and often grows over the cornea to cause blurry or cloudy vision. Pterygiums tend to occur more frequently in tropical climates and among people who spend considerable time outdoors; both eyes may be affected. Although its cause remains unknown, long-term sun exposure is believed to play a part.
Your doctor can diagnose pterygium by conducting a comprehensive eye exam, using special instruments. He or she may recommend eye drops to alleviate dryness and irritation as well as ointments or gels that inhibit new tissue from growing. In extreme cases, surgery may be advised – autologous conjunctival autografting has proven the lowest recurrence rate among all available methods of surgery.
2. Allergic Conjunctivitis
An allergic conjunctivitis is an inflammation of the clear mucus membrane that lines inner eyelids and covers the white part of an eyeball (known as the sclera). It may occur seasonally due to environmental allergens like pollen or mold spores; or year-round due to indoor allergens like dust mites and pet dander; neither form are contagious.
Symptoms may include itchy eyes, watery or red eyes and puffy lids. It is essential to identify and avoid allergens that trigger such reactions in order to stop further episodes of symptoms from recurring.
Treatment includes antihistamine eye drops and ointments to ease itchy eyes and redness, mild eye steroid drops to reduce inflammation and decrease discharge, mast cell stabilizers for more severe reactions and prednisone for preventative purposes. These drugs should ideally be taken prior to exposure of allergens so as to minimize allergic responses.
3. Macular Degeneration
Macular Degeneration (MD) is a progressive eye condition in which central retina (or “macula”) degeneration results in vision loss in one or both eyes, impairing driving ability, threading needles accurately, reading books and recognising faces among other activities. Central vision is essential for driving safely, threading needles correctly, reading aloud and recognising people in faces.
These symptoms of macular degeneration include gradual vision deterioration, difficulty in recognizing faces or objects, needing brighter lights for tasks, wavy or crooked lines when looking at straight objects such as books or roads, as well as wavy or crookedness when viewing straight lines like books or roads. It is a widespread eye condition affecting both eyes.
Macular degeneration can be divided into dry and wet forms. The former causes tissue to thin beneath the retina around the macula area and begins with yellow deposits known as drusen that eventually break down, while wet macular degeneration occurs when abnormal blood vessels leak fluid under the retina, leading to rapid vision loss and possibly treatment by means of vitamin therapy or increased consumption of green, leafy vegetables.
4. Retinal Detachment
Retinal detachment occurs when the retina detaches from its support structure in the eyeball and cannot receive its blood supply, making proper functioning impossible. Therefore, prompt treatment must be sought immediately in order to avoid complete loss of vision.
The retina is the inner lining of our eye that converts light to electrical signals for our brain to interpret into images we perceive. When detached, this causes blurred and distorted vision; symptoms include sudden floaters or black curtains or shadows moving across or blocking parts of peripheral or central vision.
Retinal detachments require prompt treatment in order to restore sight, and vitrectomy may be the necessary remedy. Vitrectomy involves pushing fluid out through a small incision in order to provide a clear view of the detaching retina and restore visibility.
5. Glaucoma
Glaucoma is an eye disease that can lead to irreparable vision loss and blindness, when the pressure in the eye increases. Aqueous humor continuously circulates within the front section of eyes providing nourishment to various parts of eye before draining off through trabecular meshwork – any blockages in this drainage area increase eye pressure significantly.
Pressure buildup on the optic nerve can damage its tissues and result in gradual vision loss, starting with peripheral vision impairment. Elderly people, African-Americans and those with family histories of optic neuritis are at an increased risk.
Astigmatism can be identified through an eye exam using tonometry, visual field testing and corneal pachymetry measurements of cornea thickness; treatment options include medications and surgical correction.
6. Cystoid Macular Edema
Macula cysts occur when fluid collects in one or more cyst-like structures in the macula, which is responsible for central (detail) vision and can result in blurred and distorted visual images. They may be caused by macular degeneration, diabetic retinopathy, retinal vein occlusion and eye injury or surgery among many other conditions.
Symptoms include blurry or distorted central visual field and mobile light streaks known as floaters which appear like cobwebs, dust or insects swarming about. Treatment options include medications like dorzolamide or Cosopt which have proven their efficacy at treating macular edema.
Subtype of Retinitis Pigosa that starts in the mid-periphery instead of typically progressing closer to vascular arcades and sparing central vision, typically through mutation in RP9 gene and linkage analysis suggests it’s non-allelic.
7. Choroidal Neovascularization
Choroidal neovascularization is the most severe form of late age-related macular degeneration, characterized by abnormal blood vessel growth in the choroid layer that leak fluid and disrupt vision. This condition is sometimes referred to as exudative or “wet” age-related macular degeneration, and can be distinguished from other types of macular degeneration by having well-demarcated areas of fluid accumulation on fluorescein angiography.
CNV can cause symptoms including distortion or blurriness of vision, dark spots in the center of vision and increased light sensitivity (photophobia). Treatment options may include laser photocoagulation or surgery. A drug inhibiting RUNX1 may help combat aberrant angiogenesis associated with proliferative diabetic retinopathy and CNV. CT scan: This advanced X-ray machine captures cross-sectional images of eye structures revealing details not visible via regular X-ray machines.
8. Pseudoexfoliation Syndrome
Pseudoexfoliation syndrome is an age-related, systemic condition characterized by depositions of fibrillar material in tissues throughout the body and specifically anterior eye structures. About 50 percent of those suffering from pseudoexfoliation syndrome will eventually progress to secondary open-angle glaucoma, which typically involves higher mean IOP levels, more rapid diurnal pressure fluctuations and damage progression than primary open-angle glaucoma.
PEX can cause white, flaky deposits on the front parts of eyes (especially lenses and structures surrounding pupil) that can be seen during slit lamp examination.
Patients diagnosed with this condition require careful and diligent adherence to treatment, including medications. When medical treatments do not work, laser trabeculoplasty may be more successful – it should preferably be conducted under sedation so the patient does not experience pain during this procedure – this service is provided by many eye centers and hospitals to their patients.
9. Pseudotumor
Pseudotumor cerebri, or false brain tumor syndrome, is a condition in which there is high pressure in the cerebrospinal fluid surrounding the brain. CSF protects and transports nutrients and waste throughout your body’s systems – typically this drains back out through your skull into the blood stream naturally but in this condition it doesn’t drain as effectively, leading to increased pressure inside of the skull and building up pressure inside it.
This can cause swelling of the optic disc at the back of the eye and vision problems. In severe cases, the patient may develop headaches and loss of consciousness.
Diagnosis can be obtained with either a lumbar puncture or MRI to measure the pressure of CSF in your skull, and treatments include taking diuretics to increase frequency of urination and relieve body fluid pressure; or performing an opthene sheath fenestration procedure which drains excess CSF through making small holes in membrane surrounding optic nerve (opthene sheath fenestration), usually providing relief of symptoms.
10. Photopsias
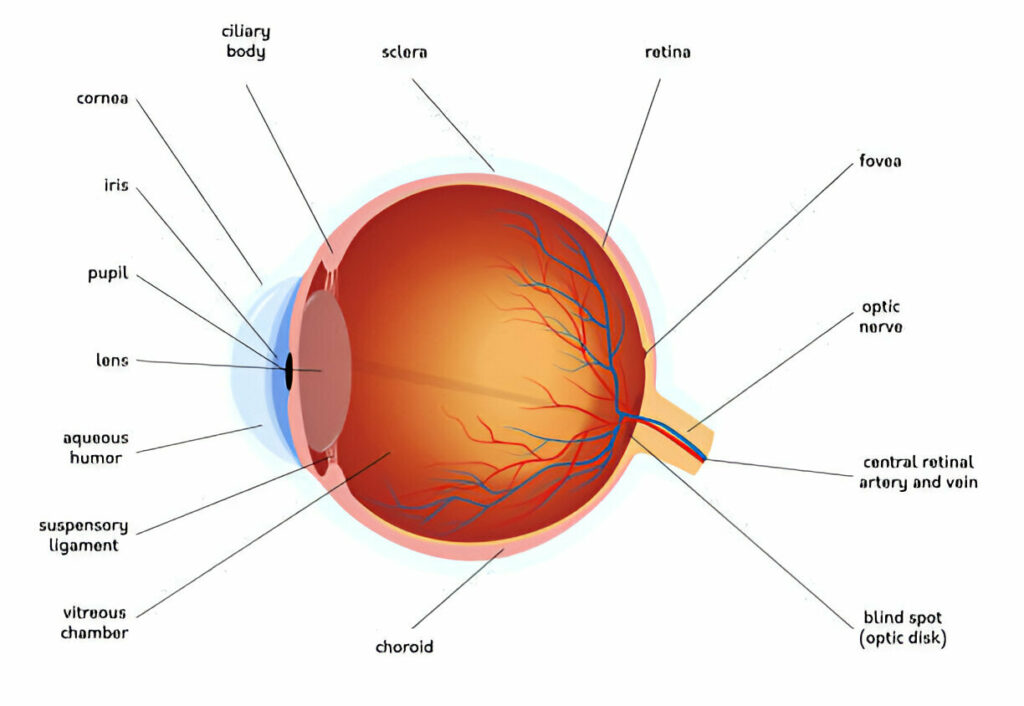
Human eyes are complex organs designed to allow humans to see. Filled with clear jelly-like substance called vitreous that allows light to travel from retina at the back of eyeball through pupil and iris until reaching retina at back. Lens helps focus incoming light onto retina. Returned light then converts to electrical signals transmitted back through optic nerve and on to brain via optic nerve.
Photopsias are flashes of light that occur spontaneously within the retina. They may take the form of lightning flashes, cobweb-like filaments or multiple floaters due to vitreous hemorrhage at retinal tears; when adhesions surrounding these tears are released the photopsia phenomenon passes quickly without lasting visual loss.